

The shoulder is a complex anatomic structure that allows movement in many planes. Patients often ignore the importance of the shoulder joint until its function becomes compromised. It then becomes obvious how crucial it is for many essential activities. The expression “If you don’t use it, you lose it” applies perfectly to diseases of the shoulder because any voluntary or involuntary guarding of the shoulder may result in loss of mobility.
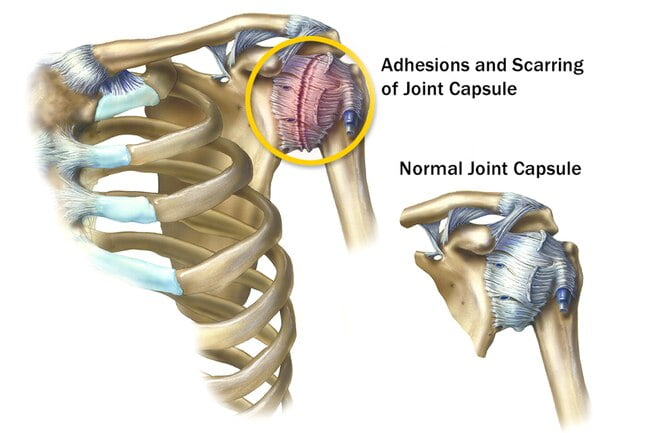
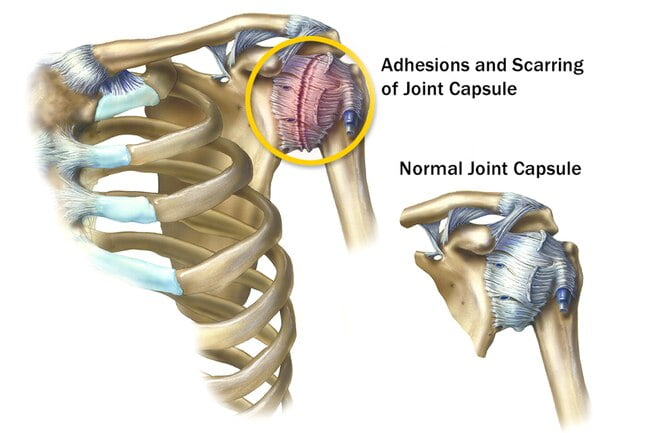
Your shoulder is made up of three bones that form a ball-and-socket joint. There’s also tissue surrounding your shoulder joint that holds everything together. This is called the shoulder capsule.
The term “adhesive capsulitis” has been applied to conditions when the shoulder is working at less than its optimal range. Because the shoulder joint is so complex, it is important to determine the precise cause for loss of shoulder mobility. It is paramount that physicians use proper terminology so that they can communicate effectively and treat patients appropriately.
What is Adhesive Capsulitis?
Adhesive Capsulitis, also called Frozen Shoulder, is a painful condition in which the movement of the shoulder becomes limited.
Adhesive Capsulitis occurs when the strong connective tissue surrounding the shoulder joint (called the shoulder joint capsule) become thick, stiff, and inflamed. (The joint capsule contains the ligaments that attach the top of the upper arm bone [humeral head] to the shoulder socket [glenoid], firmly holding the joint in place. This is more commonly known as the “ball and socket” joint.)
The condition is called “frozen” or “Adhesive” shoulder as it becomes stiff, because the more pain that is felt, the less likely the shoulder will be used. Lack of use causes the shoulder capsule to thicken and becomes tight, making the shoulder even more difficult to move — it is “frozen” in its position.
Aetiology/Causes:
- The bones, ligaments and tendons that make up your shoulder joint are encased in a capsule of connective tissue. Frozen shoulder occurs when this capsule thickens and tightens around the shoulder joint, restricting its movement.
- Presently doctors being unclear for this condition. although it’s more likely to occur in people who have diabetes or those who recently had to immobilize their shoulder for a long period.
- The pathos-aetiology of adhesive capsulitis is, however, complex and multifactorial with both geneticand environmental factors playing an important role.
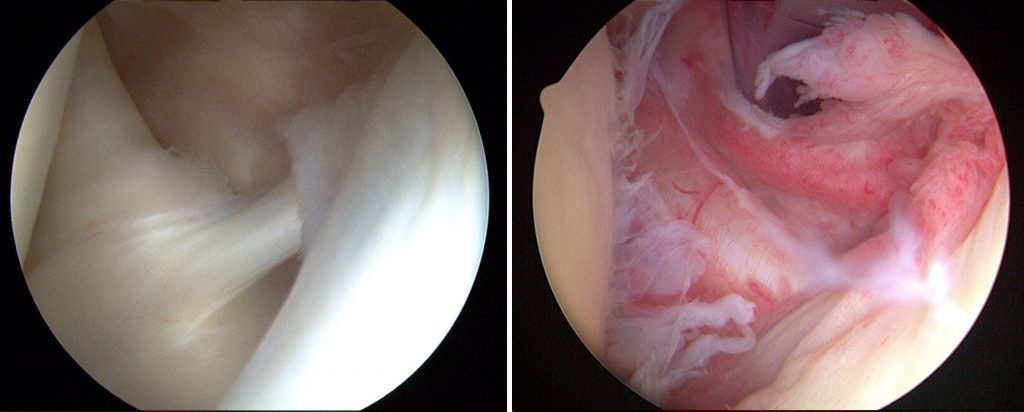
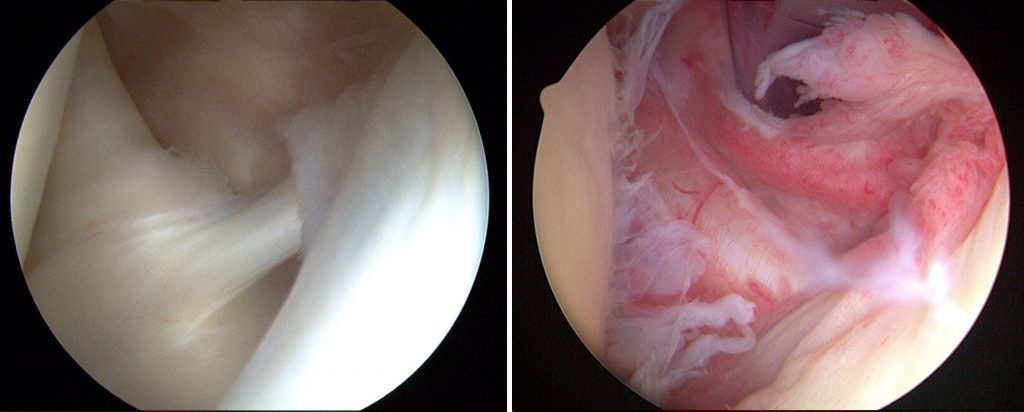
- However, there is a hypothesis based on arthroscopic and pathologic observations, that there is an inflammatory component within the axillary fold. This is followed by stiffness and adhesions, which results in fibrosis of the synovial lining, which is associated with the inflammation.
Hence there are two categories for the adhesive capsulitis/ Frozen Shoulder:
- Primary– Onset is generally idiopathic (it comes on for no attributable reason).
- Secondary– Results from a known cause, predisposing factor or surgical event. For example, post-surgery, post-stroke and post-injury, an arm fracture.
Where post-injury, there may be an altered movement patterns to protect the painful structures, which will in turn change the motor control of the shoulder, reducing the range of motion, and gradually stiffens up the joint.
Three subcategories of secondary frozen shoulder include:
- Systemic(diabetes mellitus and other metabolic conditions);
- Extrinsic factors(cardiopulmonary disease, cervical disc, CVA, humerus fractures, Parkinson’s disease);
- Intrinsic factors(rotator cuff pathologies, biceps tendinopathy, calcific tendinopathy, AC joint arthritis).
People 40 and older, particularly women, are more likely to have frozen shoulder.
Incidence:
Adhesive capsulitis has an incidence of 3–5% in the general population and up to 20% in those with diabetes. This disorder is one of the most common musculoskeletal problems seen in orthopaedics .Although some have described adhesive capsulitis as a self-limiting disorder that resolves in 1–3 years other studies report ranges of between 20 and 50% of patients with adhesive capsulitis which suffer long-term range of motion (ROM) deficits that may last up to 10 years .
The typical patient that develops adhesive capsulitis is a female in her 5th to 7th decade of life. Adhesive capsulitis is commonly associated with other systemic and no systemic conditions. By far the most common is the co-morbid condition of diabetes mellitus, with an incidence of 10–36% .
Other co-morbid conditions include hypoadrenalism, Parkinson’s disease, hyperthyroidism, pulmonary disease, hypothyroidism, cardiac disease, stroke, and even surgical procedures that do not affect the shoulder such as cardiac surgery, cardiac catheterization, neurosurgery, and radical neck dissection.
Symptoms:
Frozen shoulder typically develops slowly, and in three stages. Each stage can last a number of months.
- The “freezing” stage.Any movement of your shoulder causes pain, and your shoulder’s range of motion starts to become limited. In this stage, the shoulder becomes stiff and is painful to move. The pain slowly increases. It may worsen at night. Inability to move the shoulder increases. This stage lasts 6 weeks to 9 months.
- The “frozen” stage:Pain may begin to diminish during this stage. However, your shoulder becomes stiffer, and using it becomes more difficult. During frozen stage pain may lessen, but the shoulder remains stiff. This makes it more difficult to complete daily tasks and activities. This stage lasts 2 to 6 months.
- The “thawing” (recovery) stage: The range of motion in your shoulder begins to improve. In this stage, pain lessens, and ability to move the shoulder slowly improves. Full or near full recovery occurs as normal strength and motion return. The stage lasts 6 months to 2 years.
Prevention:
- One of the most common causes of frozen shoulder is the immobility that may result during recovery from a shoulder injury, broken arm or a stroke. If you’ve had an injury that makes it difficult to move your shoulder, talk to your doctor about exercises you can do to maintain the range of motion in your shoulder joint.
However Adhesive capsulitis is a musculoskeletal condition that has a disabling capability. The early diagnosis can be cured with non-operative treatments. But if the condition is ignored for the long time it can be turned into serious one which has to go under operative management for recovery.
1,312 comments to “Adhesive Capsulitis: A Sticky Issue”
Great blog here! Also your site loads up very fast!
What web host are you using? Can I get your affiliate link to
your host? I wish my web site loaded up as fast as yours lol
I was recommended this web site by my cousin. I am not sure whether this post is written by
him as nobody else know such detailed about my trouble.
You are incredible! Thanks!
Thank you for another great article. Where else may anyone get that kind of information in such an ideal approach of writing?
I’ve a presentation next week, and I’m on the look for such
information.
whoah this weblog is fantastic i love reading your posts.
Stay up the great work! You already know,
a lot of persons are looking around for this information, you could help them greatly.
I’m not sure why but this weblog is loading very slow for me.
Is anyone else having this problem or is it a issue on my end?
I’ll check back later and see if the problem still exists.
You are so awesome! I don’t think I have read something like that before.
So wonderful to find somebody with original thoughts on this subject.
Really.. thank you for starting this up. This website
is one thing that is required on the web, someone with a little originality!
I believe this is among the such a lot important info for me.
And i’m glad studying your article. But wanna statement on few normal issues, The website style
is wonderful, the articles is in reality excellent : D.
Excellent process, cheers
I’m truly enjoying the design and layout of your blog.
It’s a very easy on the eyes which makes it much more enjoyable for me
to come here and visit more often. Did you hire
out a designer to create your theme? Superb work!
Attractive section of content. I just stumbled upon your blog and in accession capital to assert that
I acquire in fact enjoyed account your blog posts.
Anyway I will be subscribing to your feeds and even I achievement you access consistently rapidly.
Wonderful beat ! I would like to apprentice while you
amend your website, how could i subscribe for a
blog web site? The account aided me a acceptable deal.
I had been tiny bit acquainted of this your broadcast provided bright clear idea
It’s remarkable to visit this web site and reading the views of all colleagues regarding this article, while I am also zealous
of getting experience.
Oh my goodness! Awesome article dude! Thank you
so much, However I am encountering troubles with your RSS.
I don’t understand why I cannot subscribe to it.
Is there anybody else getting identical RSS problems?
Anybody who knows the answer can you kindly respond?
Thanks!!
Hi there very cool web site!! Guy .. Beautiful .. Amazing ..
I will bookmark your web site and take the feeds also?
I am happy to search out a lot of useful info here in the publish, we need develop extra strategies in this regard,
thanks for sharing. . . . . .
I was curious if you ever thought of changing the structure of
your website? Its very well written; I love what youve got to
say. But maybe you could a little more in the way of content
so people could connect with it better. Youve got an awful lot of
text for only having one or two images. Maybe you could space
it out better?
I’ll immediately grasp your rss feed as I can’t to find your email subscription hyperlink or newsletter service.
Do you’ve any? Kindly permit me know so that I could subscribe.
Thanks.
Thanks for finally writing about > Adhesive Capsulitis: A Sticky Issue – Agile Ortho < Loved it!
Hi! Do you use Twitter? I’d like to follow you if that
would be okay. I’m undoubtedly enjoying your blog and
look forward to new updates.
Excellent article. I absolutely appreciate this site.
Continue the good work!
Great beat ! I would like to apprentice while you amend your website, how can i subscribe for a blog website?
The account aided me a acceptable deal. I had been a little bit acquainted
of this your broadcast provided bright clear concept
Good day! This post couldn’t be written any better!
Reading this post reminds me of my previous room mate!
He always kept chatting about this. I will forward this post to him.
Pretty sure he will have a good read. Thanks for sharing!
Wonderful blog! I found it while searching on Yahoo News.
Do you have any suggestions on how to get listed
in Yahoo News? I’ve been trying for a while but I never
seem to get there! Many thanks
It has a massive variety of slots, the best table games, and
HD reside dealer games.
precursor was “twenty-one,” a game of unknown origin, but references to this game have been initially
An outstanding share! I have just forwarded this onto a coworker who had been doing a little research on this. And he in fact bought me breakfast because I discovered it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanks for spending some time to talk about this issue here on your blog.
Have you ever considered publishing an e-book or guest authoring on other websites?
I have a blog centered on the same subjects you discuss and
would love to have you share some stories/information. I
know my subscribers would appreciate your work. If you are even remotely interested, feel free
to shoot me an e mail.
Howdy very cool website!! Guy .. Excellent .. Wonderful ..
I will bookmark your blog and take the feeds additionally?
I’m satisfied to find so many useful information right here within the publish,
we want work out more strategies on this regard, thank you for
sharing. . . . . .
you are actually a good webmaster. The website loading velocity is amazing.
It kind of feels that you’re doing any distinctive
trick. Also, The contents are masterpiece. you’ve performed a excellent task in this subject!
I used to be recommended this blog via my cousin. I am not positive whether this submit is written via him as no one else understand
such certain approximately my problem. You are amazing!
Thank you!
Hi there just wanted to give you a quick heads up.
The text in your article seem to be running off the screen in Opera.
I’m not sure if this is a format issue or something to do with browser compatibility
but I figured I’d post to let you know. The design and style look great though!
Hope you get the issue resolved soon. Thanks
You actually make it seem so easy with your presentation but I
find this topic to be actually something which I think I would never understand.
It seems too complicated and extremely broad for me. I am looking forward for
your next post, I will try to get the hang of it!
I every time emailed this website post page to all my associates, as if
like to read it next my links will too.
Hi! Would you mind if I share your blog with my facebook
group? There’s a lot of folks that I think would really
enjoy your content. Please let me know. Cheers
Hello! I could have sworn I’ve been to this site before but after checking through some of the post I realized it’s new to me.
Nonetheless, I’m definitely glad I found it and I’ll be
book-marking and checking back frequently!
whoah this blog is wonderful i really like reading your articles.
Keep up the good work! You realize, lots of individuals are hunting round for this information, you could help them greatly.
I think the admin of this website is really working hard in favor of
hiss web site, as here evey material is quality basrd material.
Here is my page: Learn here
The following sections are about several popular match bonus promotions.
My webpage; Learn here
Thanks for finally talking about > Adhesive Capsulitis:
A Sticky Issue – Agile Ortho < Liked it!
Apart from all this, earlier than hiring any marriage ceremony music band you
must take suggestion from your associate. The band was comprised of
her household and she was the lead singer. However, her
parents needed her to be part of the band and she
had no choice. For many who grew up in the 90s, pop-punk was the
sound of the time and was a significant a part of our reminiscences for
many years to come. The pair, who lived and worked in Victorian London, produced 14 light operas collectively.
These embrace “The Pirates of Penzance,” “The Mikado” and “H.M.S. Pinafore,” all of which are still produced and enthusiastically attended immediately.
Karaoke recordsdata are quite a lot of songs out there by the
use of music recordsdata that you receive to your computer.
What have been your favourite songs? When you consider the
’80s, this may be certainly one of the first songs to return to thoughts.
For building an attention-grabbing and highly responsive application, it’s good to develop two completely different modules: one for drivers
and one for passengers.
BetOnline has operated for over 25 years and is a properly-established brand.
There is a no-deposit bonus of 25 Absolutely free Spins if
you register for a absolutely free account.
I’d like to find out more? I’d love to find
out more details.
If some one desires to be updated with hottest technologies therefore he must be visit this web site and be up to date everyday.
RTP stands for Return to Player, and higher RTP is an indication of how substantially chance a player has to
win.
We’re a group of volunteers and opening a new scheme in our community.
Your web site provided us with valuable information to work on. You’ve done an impressive job and our entire community
will be thankful to you.
You ought to be a part of a contest for one of the highest quality sites on the web.
I am going to highly recommend this blog!
With Paysafecard casinos, you never ever expose your bank information to the actual casinos generating it one hundred% secure.
Thanks to this blog, I’ve turn into a better pet owner and have even connected with other pet lovers
who share my passion.
Sports Guru Pro India vs PAK normally getting very anticipated.
It helps you to acquire backlinks thereby boosting your blog’s Search engine optimisation and authority.
Now, build a blank page on your blog and title it “Privacy Policy”.
To winn the jackpot, you need to get all 5 numbers correct, aas properly as the Megga
Ball number.
Also visit my blog post: ga lottery
Regular expressions of love and appreciation contribute to
a positive and uplifting atmosphere.
I have been exploring for a little bit for any high-quality articles or blog posts in this sort of area .
Exploring in Yahoo I at last stumbled upon this web site.
Studying this info So i’m satisfied to show that I’ve an incredibly just right uncanny feeling I came upon just what I needed.
I most for sure will make sure to do not overlook
this site and give it a look on a constant basis.
Nice blog here! Also your website loads up fast!
What host are you using? Can I get your affiliate link to
your host? I wish my web site loaded up as fast as yours lol
Hi there exceptional website! Does running a blog similar to this take a
lot of work? I have absolutely no expertise in coding but I was hoping to start my own blog soon. Anyways, should you have any suggestions or tips for
new blog owners please share. I understand this is off topic nevertheless I just wanted to ask.
Appreciate it!
Good way of telling, and nice piece of writing to obtain information regarding my presentation subject matter, which
i am going to present in institution of higher education.
Very rapidly this web page will be famous among all blogging and site-building visitors, due to it’s pleasant articles or reviews
Wonderful blog! I found it while browsing on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo
News? I’ve been trying for a while but I never seem to get there!
Thanks
Upstart is a lending marketplace featuring a network of provate loan providers that cater to
borrowers with no credit score or a restricted financial history.
my web blog legit online loans guaranteed approval
Woah! I’m really enjoying the template/theme of this site.
It’s simple, yet effective. A lot of times it’s very difficult to get that “perfect balance” between superb
usability and appearance. I must say that you’ve done a very good job with this.
Additionally, the blog loads very fast for me on Chrome.
Excellent Blog!
The SBA offers a wealth oof resources to help modest company owners.
Have a look at my site :: loan places near me
This is very interesting, You’re an overly skilled blogger.
I have joined your feed and look forward to searching for
more of your great post. Additionally, I’ve shared
your website in my social networks
Coupon interest payments occur at predetermined intervals, generally annually
or semi-annually.
Also visit my website; online loans with monthly payments
Wow! At last I got a weblog from where I be able to truly
get helpful information regarding my study and knowledge.
Nonetheless, some other installment loan offerings have a maximum APR of 35.99%,
depending on the applicant’s credit history.
My website online loans with monthly payments
I always spent my half an hour to read this webpage’s posts every day along with a cup of coffee.
Appreciation to my father who stated to me regarding this web site, this
weblog is actually amazing.
You’ve made some good points there. I looked on the internet for additional information about the issue and found most people will go along with your
views on this site.
Woah! I’m really enjoying the template/theme of this site.
It’s simple, yet effective. A lot of times it’s tough
to get that “perfect balance” between user friendliness and visual appearance.
I must say you’ve done a excellent job with this.
In addition, the blog loads extremely quick for me on Firefox.
Exceptional Blog!
Superb blog! Do you have any hints for aspiring
writers? I’m planning to start my own blog soon but I’m a little lost on everything.
Would you recommend starting with a free platform like WordPress or go for a paid option? There are so
many choices out there that I’m totally overwhelmed ..
Any ideas? Bless you!
Hello, I enjoy reading all of your post. I wanted to write a little comment
to support you.
whoah this weblog is great i love reading your articles.
Keep up the great work! You recognize, a lot of persons are hunting round for this information, you can help them
greatly.
Excellent website. Plenty of helpful information here. I’m sending it to several
pals ans also sharing in delicious. And naturally, thank you on your effort!
I quite like reading an article that will make men and women think.
Also, thank you for permitting me to comment!
Hey there! Would you mind if I share your blog with my twitter group?
There’s a lot of folks that I think would really appreciate your content.
Please let me know. Thanks
For most recent news you have to pay a visit
web and on world-wide-web I found this website as a finest web site for hottest
updates.
Hi there Dear, are you truly visiting this website regularly, if so after that you will
definitely obtain good experience.
I’m impressed, I must say. Rarely do I come across a blog that’s both educative and engaging, and let me
tell you, you’ve hit the nail on the head. The
problem is something not enough men and women are
speaking intelligently about. I’m very happy I stumbled across this in my search for something relating to this.
branded itself the “King of Parlays,” centered
Most supply a matched deposit bonus that can be utilised in the sportsbook.
There is an inherent energy struggle between applications and base layers.
Greate post. Keep posting such kind of info on your page.
Im really impressed by your site.
Hey there, You have performed an excellent job.
I will certainly digg it and in my opinion recommend to my
friends. I’m sure they will be benefited from this website.
Hi there just wanted to give you a quick heads up and let
you know a few of the pictures aren’t loading correctly. I’m not sure why but I think its a linking issue.
I’ve tried it in two different browsers and both show the same
outcome.
I want to to thank you for this good read!! I certainly enjoyed every little bit of it.
I have got you saved as a favorite to check out new things you post…
Hey There. I found your blog using msn. This is
a very well written article. I’ll be sure to bookmark it and return to read more of your useful info.
Thanks for the post. I’ll definitely return.
Right away I am going to do my breakfast, afterward having my breakfast coming over again to read
other news.
obviously like your website however you have to check the
spelling on quite a few of your posts. Several of them are rife with spelling problems and I to find it very bothersome to inform the truth on the other hand I will definitely come again again.
Yes! Finally someone writes about krucil.
whoah this weblog is great i love reading your posts.
Stay up the good work! You understand, many persons are looking around for this info, you
could aid them greatly.
Very great post. I simply stumbled upon your blog and wished to say
that I’ve truly enjoyed surfing around your weblog posts. After all I will be subscribing on your rss
feed and I’m hoping you write again very soon!
You made some good points there. I looked on the internet to learn more about the issue and found
most people will go along with your views on this site.
Howdy just wanted to give you a quick heads up and let you know a few of
the images aren’t loading properly. I’m not sure
why but I think its a linking issue. I’ve tried it in two
different web browsers and both show the same results.
It’s perfect time to make a few plans for the long run and it is time to be happy.
I have read this post and if I could I desire to recommend you few attention-grabbing issues or
suggestions. Perhaps you could write subsequent articles relating to this article.
I desire to read even more things approximately it!
hey there and thank you for your information –
I have certainly picked up anything new from right here.
I did however expertise some technical issues using this site, as I experienced to reload the site many times previous
to I could get it to load properly. I had been wondering if your web host is OK?
Not that I am complaining, but sluggish loading instances times will sometimes affect
your placement in google and can damage your quality
score if advertising and marketing with Adwords.
Well I’m adding this RSS to my e-mail and could look out for a lot more of your respective interesting content.
Ensure that you update this again very soon.
Because the admin of this web site is working, no question very quickly it will be renowned, due to its quality contents.
It’s an amazing paragraph for all the web users; they will take benefit from it I am sure.
Thank you for every other excellent article. The place else could
anyone get that kind of info in such an ideal manner of writing?
I’ve a presentation next week, and I am at the search for such information.
Have you ever thought about publishing an ebook
or guest authoring on other websites? I have a blog based on the same ideas you discuss and would love to
have you share some stories/information. I know my
audience would enjoy your work. If you’re even remotely interested,
feel free to send me an e-mail.
Just desire to say your article is as amazing. The clearness in your post is just nice and i could assume you are an expert on this subject.
Fine with your permission allow me to grab your RSS feed to
keep up to date with forthcoming post. Thanks a
million and please carry on the rewarding work.
Hello everyone, it’s my first go to see at this web site,
and article is genuinely fruitful designed
for me, keep up posting such content.
Hi every one, here every one is sharing such familiarity, thus it’s good
to read this webpage, and I used to visit this blog every day.
I blog quite often and I genuinely thank you for your information. This article has truly peaked my
interest. I am going to take a note of your site
and keep checking for new details about once per week. I subscribed to your RSS feed as well.
Amazing blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple tweeks would really make my blog jump out.
Please let me know where you got your design. With thanks
Wow, wonderful blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your
web site is fantastic, let alone the content!
I’m not that much of a online reader to be honest but your sites really
nice, keep it up! I’ll go ahead and bookmark your website to
come back down the road. Many thanks
Wonderful goods from you, man. I have understand your
stuff previous to and you’re just extremely excellent.
I really like what you’ve acquired here, really like what you are
saying and the way in which you say it. You make it entertaining and you still take care of to keep it sensible.
I cant wait to read far more from you. This is really a tremendous web
site.
WOW just what I was looking for. Came here by searching for
forum igo dewasa
Hello there, just became aware of your blog through Google,
and found that it’s really informative. I’m gonna watch out for brussels.
I’ll be grateful if you continue this in future.
A lot of people will be benefited from your writing.
Cheers!
Ahaa, its fastidious discussion regarding this piece of writing here at this blog, I have read all that, so at this time me also commenting here.
Helpful info. Lucky me I found your site by chance,
and I am surprised why this accident did not happened earlier!
I bookmarked it.
Hi there, I read your new stuff regularly. Your writing style is witty, keep doing what you’re doing!
Hi there to all, since I am truly eager of reading
this webpage’s post to be updated regularly.
It includes good stuff.
Hi there i am kavin, its my first time to commenting anyplace, when i read
this article i thought i could also create comment due to this sensible piece
of writing.
I feel this is one of the such a lot significant information for me.
And i am satisfied reading your article. However should observation on some general things, The web site style
is wonderful, the articles is in point of fact great :
D. Good activity, cheers
My spouse and I stumbled over here by a different page and thought I might as
well check things out. I like what I see so now
i am following you. Look forward to exploring your web page yet again.
This post is invaluable. When can I find out more?
I’m not that much of a internet reader to be honest but your blogs really nice, keep it up!
I’ll go ahead and bookmark your site to come back later
on. Many thanks
Excellent website. Lots of useful info here.
I am sending it to a few friends ans additionally sharing in delicious.
And obviously, thanks in your effort!
Definitely believe that which you stated. Your favorite justification seemed to be on the web the easiest thing to
be aware of. I say to you, I certainly get irked
while people consider worries that they plainly don’t know about.
You managed to hit the nail upon the top and defined out the whole thing without having side-effects , people can take a signal.
Will likely be back to get more. Thanks
Pretty component of content. I just stumbled upon your weblog and
in accession capital to say that I get actually loved account your blog posts.
Any way I’ll be subscribing on your augment and even I fulfillment you get admission to constantly rapidly.
Its like you learn my thoughts! You appear
to understand so much approximately this, such as you wrote the book in it or something.
I feel that you just can do with some p.c. to power the message house a bit, however instead of that,
that is great blog. An excellent read. I’ll certainly be back.
Link exchange is nothing else except it is just placing the other person’s weblog link on your page at suitable place
and other person will also do same in favor of you.
I have fun with, result in I found just what I was taking a look
for. You’ve ended my four day long hunt! God Bless you man. Have
a great day. Bye
Hi, i think that i saw you visited my website so i came to “return the favor”.I’m trying to find things to enhance my website!I suppose its ok to use
a few of your ideas!!
Inspiring quest there. What occurred after? Good luck!
Great blog! Do you have any helpful hints for aspiring writers?
I’m planning to start my own blog soon but I’m a
little lost on everything. Would you propose starting with a free platform like WordPress or go for a paid
option? There are so many options out there that I’m
totally overwhelmed .. Any tips? Appreciate it!
Hello there! This is my first visit to your blog! We
are a team of volunteers and starting a new initiative in a community in the same niche.
Your blog provided us useful information to work on. You have done a
extraordinary job!
I loved as much as you’ll receive carried out right here.
The sketch is attractive, your authored subject matter
stylish. nonetheless, you command get got an nervousness over that you
wish be delivering the following. unwell unquestionably come further formerly again as exactly the same nearly
very often inside case you shield this hike.
What a data of un-ambiguity and preserveness of precious familiarity on the topic of unexpected feelings.
Hi there, I found your site by way of Google whilst searching for a similar matter,
your website got here up, it seems good.
I have bookmarked it in my google bookmarks.
Hi there, simply changed into alert to your weblog through Google, and found that it’s truly
informative. I am going to watch out for brussels. I’ll appreciate in case you proceed this in future.
A lot of folks will probably be benefited from your writing.
Cheers!
Oh my goodness! Incredible article dude! Many thanks, However I am encountering troubles with your RSS.
I don’t understand the reason why I am unable to join it. Is there anybody getting similar RSS issues?
Anybody who knows the answer can you kindly respond?
Thanks!!
This text is priceless. Where can I find out more?
It’s not my first time to pay a visit this website, i am visiting
this web page dailly and take pleasant facts from
here daily.
Hi my family member! I wish to say that this post is amazing, nice written and include approximately all significant infos.
I would like to look more posts like this .
Highly descriptive blog, I enjoyed that bit.
Will there be a part 2?
Unquestionably consider that that you stated. Your favorite reason appeared to be on the web the easiest factor to take into
account of. I say to you, I definitely get annoyed whilst other people think about concerns
that they just do not recognize about. You controlled
to hit the nail upon the top as smartly as outlined out
the whole thing without having side effect , folks could take
a signal. Will probably be again to get more. Thank you
Hi there to every one, the contents present at this web site are truly amazing for people experience,
well, keep up the nice work fellows.
What a data of un-ambiguity and preserveness of valuable
experience regarding unexpected feelings.
I feel that is one of the most vital information for me. And
i’m satisfied reading your article. However should remark
on some general things, The web site taste is wonderful, the articles
is really excellent : D. Just right process, cheers
Nice answers in return of this query with solid arguments and telling everything about that.
Wonderful beat ! I wish to apprentice while you amend your site, how can i
subscribe for a blog website? The account aided me a acceptable deal.
I had been tiny bit acquainted of this your broadcast offered bright clear idea
It’s in reality a nice and useful piece of information. I’m glad
that you simply shared this useful information with us. Please keep us informed like this.
Thanks for sharing.
Simply want to say your article is as surprising.
The clarity in your post is just great and i could assume you’re an expert on this subject.
Well with your permission let me to grab your feed to keep
updated with forthcoming post. Thanks a million and please carry
on the rewarding work.
It’s actually a cool and useful piece of info. I’m happy that you
shared this helpful information with us. Please stay us up to date like this.
Thank you for sharing.
I am not sure where you are getting your info, but great
topic. I needs to spend some time learning much more or understanding more.
Thanks for excellent information I was looking for
this info for my mission.
Hello! I could have sworn I’ve visited this site before but after looking at some
of the articles I realized it’s new to me. Nonetheless, I’m certainly delighted I stumbled upon it and I’ll be book-marking it and checking back frequently!
Pretty nice post. I just stumbled upon your weblog
and wished to say that I have truly enjoyed browsing your blog posts.
After all I’ll be subscribing to your rss feed and I
hope you write again very soon!
Great post. I was checking constantly this blog and I’m impressed!
Extremely helpful information specifically the last part 🙂 I care for such information much.
I was seeking this particular info for a long time. Thank you and
good luck.
I don’t even know how I ended up here, but I thought this post was good.
I don’t know who you are but definitely you are going to a famous blogger if you are not already 😉 Cheers!
Everyone loves what you guys are up too. This type of clever work and exposure!
Keep up the superb works guys I’ve incorporated you guys to
our blogroll.
When some one searches for his necessary thing, thus he/she wishes to be
available that in detail, so that thing is maintained over here.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point.
You definitely know what youre talking about, why throw
away your intelligence on just posting videos to your blog
when you could be giving us something informative
to read?
Wow, superb blog layout! How lengthy have you ever been running
a blog for? you make blogging glance easy. The full glance of your site is excellent,
as neatly as the content!
Today, I went to the beach with my kids. I found a sea shell and gave it to my 4 year old daughter and said
“You can hear the ocean if you put this to your ear.” She placed the shell to her ear and screamed.
There was a hermit crab inside and it pinched her ear.
She never wants to go back! LoL I know this is completely off topic but I had
to tell someone!
This is the right website for anyone who really
wants to find out about this topic. You realize a whole lot its almost hard to argue with you (not that I personally will need to…HaHa).
You certainly put a fresh spin on a subject that has been discussed for years.
Wonderful stuff, just great!
Good post but I was wanting to know if you
could write a litte more on this topic? I’d be very grateful if you could elaborate a little bit further.
Cheers!
If some one desires expert view regarding running a blog after that i advise
him/her to go to see this website, Keep up the good work.
Good post. I learn something totally new and challenging on websites I stumbleupon every day.
It will always be helpful to read through articles from other authors and practice a little something
from other sites.
Good day! This is kind of off topic but I need some help
from an established blog. Is it difficult to set up your own blog?
I’m not very techincal but I can figure things out pretty
fast. I’m thinking about making my own but I’m not sure where to start.
Do you have any tips or suggestions? With thanks
I am regular visitor, how are you everybody?
This article posted at this site is really
fastidious.
Thanks designed for sharing such a good opinion,
piece of writing is nice, thats why i have
read it entirely
Wow, this post is fastidious, my sister is analyzing such things, thus I am
going to let know her.
My brother suggested I would possibly like this website.
He was totally right. This put up truly made my day. You can not consider simply how much time I had spent for this information! Thanks!
It’s great that you are getting thoughts from this post as well as from our dialogue made at this time.
I pay a visit every day some blogs and blogs to read articles
or reviews, except this webpage offers quality based content.
Simply desire to say your article is as amazing.
The clarity in your post is just cool and that i can think you’re knowledgeable
on this subject. Fine with your permission allow me to grasp your RSS
feed to stay updated with forthcoming post. Thanks a million and please keep up the rewarding
work.
Somebody essentially help to make significantly posts I would state.
That is the first time I frequented your website page and up to
now? I surprised with the research you made to create this actual
submit incredible. Wonderful activity!
We stumbled over here different website and thought I should check things out.
I like what I see so i am just following you.
Look forward to looking into your web page for a second time.
Hey there, I think your blog might be having browser compatibility issues.
When I look at your website in Opera, it looks fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up!
Other then that, awesome blog!
Asking questions are genuinely pleasant thing if you are not understanding something entirely, except this article provides
fastidious understanding even.
In fact no matter if someone doesn’t know then its up to
other users that they will assist, so here it occurs.
An outstanding share! I have just forwarded this onto
a coworker who has been doing a little research on this.
And he in fact ordered me lunch due to the fact
that I discovered it for him… lol. So allow me to reword this….
Thanks for the meal!! But yeah, thanks for spending some time to talk about this matter here on your website.
I know this if off topic but I’m looking into starting
my own weblog and was wondering what all is required to get set up?
I’m assuming having a blog like yours would
cost a pretty penny? I’m not very internet savvy
so I’m not 100% positive. Any recommendations or advice would be greatly appreciated.
Cheers
Hey, I think your blog might be having browser compatibility issues.
When I look at your website in Ie, it looks
fine but when opening in Internet Explorer, it has some overlapping.
I just wanted to give you a quick heads up!
Other then that, excellent blog!
Wow, marvelous blog layout! How long have you been running a blog
for? you make blogging glance easy. The entire look of your web
site is great, as neatly as the content!
I got this website from my friend who informed me
concerning this site and now this time I am visiting
this web site and reading very informative articles at this place.
A fascinating discussion is worth comment. I do believe that you need
to write more about this subject matter, it might not be a taboo subject but
typically people do not discuss such subjects. To the next!
Kind regards!!
It’s enormous that you are getting thoughts from this article as well as from our discussion made here.
I just could not depart your site prior to suggesting
that I actually loved the standard info an individual provide for
your visitors? Is going to be back continuously in order to check out
new posts
Greetings! Very helpful advice in this particular article!
It’s the little changes that make the most important changes.
Thanks a lot for sharing!
They all accept the South Affican Rand aand present remarkable deposit bonuses to Souyth African players.
Feel free to surf to my homepage: 우리카지노계열
It’s hard to find well-informed people for this topic, however, you
seem like you know what you’re talking about! Thanks
I love looking through an article that can make people think.
Also, many thanks for allowing for me to comment!
I have been surfing on-line more than 3 hours nowadays,
yet I by no means discovered any attention-grabbing article
like yours. It is lovely price sufficient for me.
Personally, if all web owners and bloggers made excellent content as
you probably did, the web will be much more useful than ever before.
If some one needs to be updated with newest technologies then he must be pay a visit this site and be up to date all the time.
I constantly emailed this website post page to
all my friends, as if like to read it next my links will too.
For the reason that the admin of this web site is working, no hesitation very rapidly it will be well-known, due to its
feature contents.
You’ve made some decent points there. I looked on the internet for additional information about the issue and found most people will
go along with your views on this website.
Hello! Quick question that’s totally off topic.
Do you know how to make your site mobile friendly? My
blog looks weird when viewing from my iphone 4.
I’m trying to find a theme or plugin that
might be able to correct this issue. If you have any suggestions, please share.
Thanks!
This info is invaluable. Where can I find out more?
Hello, i think that i saw you visited my site thus
i came to “return the favor”.I am attempting
to find things to improve my website!I suppose its ok to use a few of your ideas!!
Ahaa, its fastidious discussion on the topic of this article at this place at this weblog, I have read all
that, so now me also commenting at this place.
Hello there I am so thrilled I found your website, I really found
you by accident, while I was searching on Yahoo for something else, Anyhow
I am here now and would just like to say thanks a lot
for a tremendous post and a all round entertaining
blog (I also love the theme/design), I don’t have time to read through it all at the minute but I have bookmarked it and also included your
RSS feeds, so when I have time I will be back to read much more,
Please do keep up the awesome b.
Valuable information. Fortunate me I discovered your site
accidentally, and I’m stunned why this twist of fate did not happened earlier!
I bookmarked it.
I don’t even know how I ended up here, but I thought this post
was great. I do not know who you are but definitely you’re going to a famous blogger if you aren’t already ;
) Cheers!
If you desire to increase your knowledge only keep visiting
this site and be updated with the newest news posted here.
Have you ever considered publishing an ebook or guest authoring on other sites?
I have a blog centered on the same subjects you discuss
and would love to have you share some stories/information. I know my subscribers would
enjoy your work. If you are even remotely interested, feel free
to shoot me an e-mail.
Hi! This is my 1st comment here so I just wanted to give a
quick shout out and tell you I truly enjoy
reading your posts. Can you recommend any other blogs/websites/forums that cover the same topics?
Many thanks!
Hurrah! At last I got a webpage from where I know how to actually get helpful data concerning my study and knowledge.
I was recommended this blog by my cousin. I am not sure whether this post is written by him as no one else know such
detailed about my difficulty. You are amazing! Thanks!
hey there and thank you for your information – I’ve definitely picked up something new from right
here. I did however expertise a few technical points using this website, as I experienced to reload the website
many times previous to I could get it to load properly. I had
been wondering if your hosting is OK? Not that I’m complaining, but sluggish loading
instances times will very frequently affect your
placement in google and could damage your high quality score if advertising and marketing with Adwords.
Anyway I’m adding this RSS to my e-mail and can look out
for a lot more of your respective fascinating content. Make sure you update this again soon.
Appreciate this post. Will try it out.
Nice blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple adjustements would really make
my blog stand out. Please let me know where you got your theme.
Cheers
Thanks for sharing your thoughts. I really appreciate your efforts and I will be waiting for your further post thank you once again.
Wow, fantastic blog layout! How long have you
been blogging for? you make blogging look easy.
The overall look of your website is fantastic, as well
as the content!
I’m now not certain where you’re getting your
information, but good topic. I must spend some time learning much more or working out more.
Thanks for magnificent info I used to be on the lookout for this info for my mission.
Attractive section of content. I just stumbled upon your site and in accession capital to assert that I get actually enjoyed account your
blog posts. Anyway I’ll be subscribing to your feeds and even I achievement you access consistently quickly.
Today, I went to the beachfront with my kids. I found a sea
shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the
shell to her ear and screamed. There was a hermit crab inside and it pinched
her ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
I needed to thank you for this wonderful read!!
I absolutely loved every bit of it. I have you bookmarked to check out new things you post…
Excellent way of describing, and good paragraph to take information about my presentation focus, which i
am going to convey in academy.
It’s enormous that you are getting ideas from this piece of writing as well as
from our dialogue made here.
Sweet blog! I found it while surfing around on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Many thanks
Good day I am so happy I found your website, I really found you by accident, while I was looking on Aol for something
else, Anyhow I am here now and would just like to say many thanks for a remarkable post and
a all round exciting blog (I also love the theme/design), I don’t have
time to browse it all at the minute but I have saved it
and also added your RSS feeds, so when I have time I will be back to read a great deal more,
Please do keep up the awesome jo.
I relish, result in I discovered just what I
was having a look for. You’ve ended my 4 day long hunt!
God Bless you man. Have a nice day. Bye
Hmm is anyone else having problems with the pictures on this blog loading?
I’m trying to find out if its a problem on my end or if it’s the
blog. Any feed-back would be greatly appreciated.
great points altogether, you simply gained a new reader. What would you recommend
about your post that you just made a few days ago?
Any certain?
I’ve been exploring for a bit for any high-quality
articles or blog posts on this sort of space .
Exploring in Yahoo I finally stumbled upon this web site.
Studying this information So i’m happy to express
that I have an incredibly just right uncanny feeling I found out just what I needed.
I so much definitely will make sure to don?t put out of your mind this
website and provides it a glance regularly.
Great post. I used to be checking constantly this weblog and I’m impressed!
Extremely useful information particularly the remaining phase 🙂 I care for such
information much. I was seeking this particular information for a long time.
Thanks and best of luck.
I’m not sure exactly why but this site is loading extremely slow
for me. Is anyone else having this issue or is it a problem on my end?
I’ll check back later on and see if the problem still exists.
Thank you for the good writeup. It in fact was a
amusement account it. Look advanced to more added agreeable from
you! By the way, how can we communicate?
Actually no matter if someone doesn’t understand afterward
its up to other viewers that they will help, so here it happens.
I think the admin of this site is really working hard in support of his website,
for the reason that here every material is quality based stuff.
I love your blog.. very nice colors & theme. Did you design this website yourself
or did you hire someone to do it for you? Plz answer back as I’m looking to design my own blog and would like to know where u got
this from. thank you
What i do not realize is in fact how you’re no longer actually a lot more
smartly-preferred than you may be now. You are so intelligent.
You recognize thus significantly when it comes to this
matter, made me in my view believe it from numerous varied angles.
Its like men and women are not involved until it’s something to accomplish with Woman gaga!
Your own stuffs outstanding. All the time deal with it up!
I was suggested this web site by my cousin. I’m not sure whether
this post is written by him as nobody else know such detailed
about my trouble. You are amazing! Thanks!
When I originally commented I clicked the “Notify me when new comments are added” checkbox and
now each time a comment is added I get four emails with the same comment.
Is there any way you can remove people from that service?
Cheers!
Your means of explaining the whole thing in this piece of writing is genuinely fastidious, every one
can easily understand it, Thanks a lot.
I am actually delighted to read this web site posts which consists of lots of useful data, thanks
for providing these kinds of statistics.
I have read so many articles or reviews regarding the blogger lovers however
this paragraph is really a fastidious paragraph, keep it up.
What’s up, all is going sound here and ofcourse every one is sharing data, that’s truly excellent, keep up writing.
Sweet blog! I found it while browsing on Yahoo News.
Do you have any tips on how to get listed
in Yahoo News? I’ve been trying for a while but I never seem to get there!
Many thanks
Thanks in support of sharing such a good opinion,
piece of writing is fastidious, thats why i have read it completely
I do not know if it’s just me or if perhaps everyone else encountering
issues with your blog. It looks like some of the text on your content are running off
the screen. Can somebody else please comment and let me know if this
is happening to them as well? This could
be a problem with my internet browser because I’ve had this happen previously.
Appreciate it
I’ve been exploring for a little bit for any high quality articles
or weblog posts on this sort of space . Exploring in Yahoo I at last stumbled upon this website.
Reading this information So i’m satisfied to show that I’ve a very good uncanny feeling I came
upon exactly what I needed. I most indisputably will make certain to don?t fail
to remember this web site and give it a glance on a relentless basis.
I got this web page from my pal who informed me concerning this site and at the moment this time
I am browsing this site and reading very informative articles or reviews at this place.
you are in reality a good webmaster. The web site loading velocity is incredible.
It kind of feels that you’re doing any unique trick.
Furthermore, The contents are masterwork.
you’ve performed a wonderful activity on this
matter!
Can I just say what a relief to find a person that genuinely knows what they’re discussing on the internet.
You definitely realize how to bring an issue to
light and make it important. A lot more people must check this out
and understand this side of the story. I was surprised that you
aren’t more popular since you certainly possess the gift.
Pretty! This has been an extremely wonderful article.
Many thanks for providing these details.
Thanks for the good writeup. It in reality was a entertainment account
it. Glance complicated to more added agreeable from
you! However, how can we communicate?
Your method of describing all in this article is truly nice, every one be able to simply know
it, Thanks a lot.
Hi my friend! I want to say that this article is amazing, nice written and include approximately all significant infos.
I’d like to look more posts like this .
Pretty nice post. I just stumbled upon your weblog and wanted to say that I have
truly enjoyed surfing around your weblog posts. After all
I’ll be subscribing to your feed and I’m hoping you write once more very soon!
Thank you for sharing your thoughts. I really appreciate your efforts and I will be waiting for your further post thank you once
again.
Spot on with this write-up, I honestly believe this web site needs much more attention. I’ll probably
be back again to see more, thanks for the advice!
Wow, this post is pleasant, my sister is analyzing such things, so I am going to tell her.
Simply wish to say your article is as astonishing. The clarity in your post is just spectacular and that i could suppose you’re a professional in this subject.
Well with your permission allow me to take hold of your feed to
stay up to date with drawing close post. Thanks one million and please carry on the gratifying work.
Just want to say your article is as surprising. The clearness
for your submit is just spectacular and i could suppose you’re a professional in this subject.
Fine along with your permission allow me to seize your feed to
stay updated with imminent post. Thank you one million and please keep up the gratifying work.
After going over a number of the blog articles on your web page,
I seriously like your way of writing a blog. I book marked it to my bookmark site list
and will be checking back soon. Take a look at my website as well and let me know what you think.
For the reason that the admin of this web page is
working, no hesitation very rapidly it will be famous, due to its feature
contents.
Nice blog here! Also your web site quite a bit up fast!
What host are you the use of? Can I am getting your
associate link in your host? I wish my web site loaded up as quickly as yours lol
Hi, i think that i saw you visited my web site so i came
to “return the favor”.I’m trying to find things to improve my site!I suppose its ok
to use a few of your ideas!!
Very good article. I will be dealing with many of
these issues as well..
A motivating discussion is worth comment. There’s no doubt
that that you need to publish more on this subject matter,
it might not be a taboo matter but usually people do
not talk about these subjects. To the next! Cheers!!
Wow! In the end I got a weblog from where I be capable of really take helpful data regarding my study and knowledge.
hello!,I really like your writing so a lot! percentage we communicate more approximately your article on AOL?
I need a specialist on this area to solve my problem.
May be that’s you! Taking a look forward to peer you.
You made some decent points there. I looked on the net for more info about the issue and found
most people will go along with your views on this website.
Have you ever thought about writing an ebook or guest authoring on other websites?
I have a blog centered on the same subjects you discuss and would really like to have you share some stories/information. I know my viewers would enjoy your work.
If you are even remotely interested, feel free to send me an e mail.
Hi, this weekend is good designed for me, since this point in time i am reading this impressive informative paragraph
here at my home.
What’s up i am kavin, its my first time to commenting anyplace, when i read this
article i thought i could also make comment due to this good article.
These are genuinely fantastic ideas in concerning blogging.
You have touched some pleasant factors here.
Any way keep up wrinting.
I visited several web pages however the audio quality for audio
songs current at this website is actually marvelous.
Hey! Would you mind if I share your blog with my myspace group?
There’s a lot of folks that I think would really
enjoy your content. Please let me know. Thank you
Hey there! This post couldn’t be written any better! Reading this post reminds me of my old room mate!
He always kept chatting about this. I will forward this post to him.
Fairly certain he will have a good read. Thank you for sharing!
Greetings! I know this is kinda off topic nevertheless I’d figured I’d ask.
Would you be interested in exchanging links or maybe guest writing
a blog post or vice-versa? My blog addresses a lot of the same topics
as yours and I think we could greatly benefit from each other.
If you might be interested feel free to shoot me an e-mail.
I look forward to hearing from you! Superb blog by the way!
At this time I am going to do my breakfast, after having my breakfast
coming over again to read other news.
You are so interesting! I don’t think I’ve truly read
a single thing like this before. So nice to find someone with a few original thoughts on this subject matter.
Seriously.. many thanks for starting this up.
This web site is something that is required on the internet, someone with a little originality!
I got this web site from my buddy who told me regarding this web page and at the moment this time I am browsing this web page
and reading very informative articles or reviews here.
Your style is very unique compared to other people I have read stuff from.
Many thanks for posting when you have the opportunity, Guess I’ll just bookmark this
page.
Hi there, this weekend is good in favor of
me, for the reason that this time i am reading this wonderful
educational post here at my residence.
After looking over a number of the articles on your blog, I
honestly like your way of blogging. I book-marked it to my bookmark webpage list and
will be checking back soon. Please check out my website as well and tell me your opinion.
Spot on with this write-up, I absolutely feel this amazing site needs a great deal more attention.
I’ll probably be returning to see more, thanks for the advice!
Good blog post. I certainly appreciate this site. Stick with
it!
An outstanding share! I have just forwarded this onto a co-worker who has been doing a little research on this.
And he actually bought me breakfast because I discovered
it for him… lol. So allow me to reword this….
Thanks for the meal!! But yeah, thanks for spending
time to discuss this subject here on your web site.
Yes! Finally someone writes about forum lendir.
Paragraph writing is also a fun, if you know then you can write or else it is
complicated to write.
Hello! I just wanted to ask if you ever have any issues with hackers?
My last blog (wordpress) was hacked and I ended up losing many months of hard work due to no backup.
Do you have any solutions to prevent hackers?
Great delivery. Sound arguments. Keep up the amazing
work.
Howdy! Someone in my Myspace group shared this site with us so I
came to look it over. I’m definitely enjoying the information. I’m bookmarking and will be tweeting this to my
followers! Wonderful blog and outstanding design.
WOW just what I was searching for. Came here by
searching for forum lendir igo della bandung
Thanks a lot for sharing this with all people
you really understand what you’re talking about! Bookmarked.
Kindly additionally discuss with my website =). We could have a link exchange arrangement among us
I’m really enjoying the design and layout of your website.
It’s a very easy on the eyes which makes it much more
pleasant for me to come here and visit more often. Did you
hire out a developer to create your theme?
Exceptional work!
Heya! I know this is somewhat off-topic but I had to ask.
Does running a well-established website like yours require a lot of work?
I’m brand new to running a blog however I do write in my diary on a daily basis.
I’d like to start a blog so I will be able
to share my experience and feelings online. Please
let me know if you have any kind of ideas or tips for new aspiring blog
owners. Thankyou!
My spouse and I stumbled over here from a different web page and thought I might as well check things out.
I like what I see so now i’m following you.
Look forward to looking over your web page repeatedly.
What’s up, of course this article is really good and I have learned lot of things from it regarding blogging.
thanks.
This is very fascinating, You’re a very professional blogger.
I have joined your rss feed and look ahead to in quest of more of your great
post. Additionally, I have shared your web site in my
social networks
I don’t even know how I ended up right here,
but I thought this put up used to be great. I don’t
recognize who you are but certainly you’re going to a
famous blogger in the event you aren’t already.
Cheers!
Thank you for sharing your thoughts. I really
appreciate your efforts and I am waiting for your next write ups thank you once
again.
Hi, i think that i saw you visited my blog thus i got here to return the desire?.I am trying to find issues to enhance my
web site!I assume its ok to use a few of your ideas!!
I was pretty pleased to find this website. I need to to thank you
for your time for this particularly wonderful read!!
I definitely appreciated every bit of it and i also have you
bookmarked to see new stuff in your website.
whoah this weblog is excellent i really like reading your
posts. Stay up the good work! You understand,
many persons are hunting round for this information, you can aid them greatly.
Touche. Sound arguments. Keep up the amazing work.
Useful information. Lucky me I found your web site by chance, and I am surprised why this twist
of fate did not took place earlier! I bookmarked
it.
Great web site. Lots of helpful information here.
I’m sending it to several buddies ans also sharing
in delicious. And obviously, thank you in your sweat!
great points altogether, you just won a emblem new reader.
What might you recommend about your publish that you just made some days in the past?
Any certain?
I am really loving the theme/design of your blog. Do you ever run into any browser compatibility issues?
A handful of my blog audience have complained
about my site not operating correctly in Explorer but looks great in Chrome.
Do you have any ideas to help fix this issue?
I’m not sure why but this site is loading incredibly slow for me.
Is anyone else having this problem or is it a issue on my
end? I’ll check back later on and see if the problem still exists.
You actually make it seem so easy with your presentation but I find this
topic to be actually something which I think I would never understand.
It seems too complicated and extremely broad for me.
I am looking forward for your next post, I’ll try to get the hang of it!
Greetings! Very useful advice within this article!
It is the little changes that make the most important changes.
Thanks a lot for sharing!
Its like you read my mind! You seem to know a lot about this, like
you wrote the book in it or something. I think that you can do with a few
pics to drive the message home a bit, but instead of that, this is great blog.
An excellent read. I’ll definitely be back.
If some one wishes expert view about blogging then i propose him/her to visit this blog, Keep up the good job.
It’s difficult to find knowledgeable people in this particular subject,
but you seem like you know what you’re talking about!
Thanks
I’m very pleased to discover this page. I wanted to thank you for your time for this particularly fantastic read!!
I definitely savored every bit of it and I have you bookmarked to see new information in your
site.
Thank you for the auspicious writeup. It in fact was a amusement
account it. Look advanced to far added agreeable
from you! However, how can we communicate?
For most up-to-date information you have to go to see world wide
web and on web I found this site as a finest web page for latest updates.
Does your site have a contact page? I’m having
problems locating it but, I’d like to shoot you an e-mail.
I’ve got some creative ideas for your blog you might be interested in hearing.
Either way, great site and I look forward to seeing it develop over
time.
It’s very trouble-free to find out any topic on web as compared to books, as I found this post at this website.
If some one wants expert view regarding
blogging and site-building afterward i recommend him/her to pay a visit this
webpage, Keep up the fastidious job.
Hi, Neat post. There is a problem with your website in internet explorer, might test this?
IE nonetheless is the marketplace leader and a good component to people will leave out your wonderful writing due to this problem.
Greetings! I know this is kind of off topic but I was wondering which
blog platform are you using for this website? I’m getting
fed up of WordPress because I’ve had issues with hackers and I’m looking at alternatives for another platform.
I would be great if you could point me in the direction of a
good platform.
Nice post. I used to be checking constantly this weblog and I’m inspired!
Extremely helpful information specially the remaining phase 🙂 I handle such information a lot.
I used to be looking for this particular info for a very lengthy time.
Thank you and best of luck.
What’s up, all is going well here and ofcourse
every one is sharing data, that’s actually excellent, keep up writing.
Good day! Do you use Twitter? I’d like to
follow you if that would be okay. I’m definitely enjoying your blog and look forward
to new updates.
Simply wish to say your article is as surprising.
The clarity in your post is simply cool and i could assume you are an expert on this subject.
Fine with your permission let me to grab your RSS feed to keep updated with forthcoming
post. Thanks a million and please carry on the enjoyable work.
Hi there just wanted to give you a quick heads up and let you
know a few of the pictures aren’t loading correctly.
I’m not sure why but I think its a linking issue.
I’ve tried it in two different internet browsers and both show the same results.
Today, I went to the beach with my children. I found a sea shell and gave it to my 4 year old daughter and said
“You can hear the ocean if you put this to your ear.” She placed the shell to her ear
and screamed. There was a hermit crab inside and it pinched her
ear. She never wants to go back! LoL I know this
is completely off topic but I had to tell someone!
It’s perfect time to make some plans for the future and it
is time to be happy. I have learn this post and if
I may just I wish to recommend you some fascinating things or advice.
Maybe you can write next articles referring to this article.
I wish to learn more things approximately it!
continuously i used to read smaller articles
which as well clear their motive, and that is also happening
with this article which I am reading now.
Hey there! I know this is somewhat off topic but I was wondering which blog platform are you using for this site?
I’m getting tired of WordPress because I’ve had issues with hackers and I’m
looking at alternatives for another platform. I would be fantastic if you could point
me in the direction of a good platform.
I have been exploring for a bit for any high-quality articles or blog posts in this sort
of house . Exploring in Yahoo I finally stumbled
upon this web site. Reading this information So i am happy to express that I’ve a very just right uncanny feeling I discovered exactly what I needed.
I such a lot undoubtedly will make certain to don?t put out of your mind
this web site and give it a glance regularly.
My programmer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using WordPress on various websites
for about a year and am nervous about switching to another platform.
I have heard good things about blogengine.net. Is there a way I can transfer all my wordpress content into it?
Any help would be greatly appreciated!
I am actually delighted to read this weblog posts which carries
lots of useful facts, thanks for providing such data.
It’s remarkable to pay a visit this web site and reading the views of
all mates about this article, while I am also eager
of getting experience.
Hey would you mind letting me know which webhost you’re utilizing?
I’ve loaded your blog in 3 different browsers and I must say this blog loads a lot quicker then most.
Can you recommend a good internet hosting provider at a honest price?
Cheers, I appreciate it!
My developer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the costs. But he’s tryiong
none the less. I’ve been using Movable-type on several
websites for about a year and am worried about switching to another platform.
I have heard great things about blogengine.net. Is there a way I can transfer all my wordpress
content into it? Any kind of help would be greatly appreciated!
Howdy! Do you use Twitter? I’d like to follow you if that would be ok.
I’m undoubtedly enjoying your blog and look forward to new
updates.
If you wish for to improve your know-how just keep visiting this web site and be updated with
the most recent gossip posted here.
Nice post. I learn something new and challenging on sites I stumbleupon everyday.
It will always be useful to read through content from other authors and use a little something from their
websites.
I have fun with, result in I discovered exactly what I used to be having a look for.
You have ended my 4 day long hunt! God Bless you man. Have a great day.
Bye
Hi all, here every one is sharing these kinds of know-how, thus it’s
nice to read this web site, and I used to visit this web site daily.
First of all I would like to say awesome blog!
I had a quick question in which I’d like to ask if you do not mind.
I was interested to find out how you center yourself and clear your
head prior to writing. I’ve had a difficult time
clearing my mind in getting my thoughts out there.
I do enjoy writing but it just seems like the first 10 to 15 minutes are usually wasted
just trying to figure out how to begin. Any recommendations or tips?
Thanks!
Sweet blog! I found it while searching on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Many thanks
Have you ever considered writing an ebook or guest
authoring on other sites? I have a blog based upon on the same ideas you discuss and would love to have you share some
stories/information. I know my audience would enjoy your work.
If you are even remotely interested, feel free to shoot me an e-mail.
I think what you typed made a lot of sense. But, consider this, what
if you added a little information? I mean, I don’t want to tell you how to run your blog, but
suppose you added a title to possibly get people’s attention? I mean Adhesive Capsulitis: A Sticky
Issue – Agile Ortho is kinda vanilla. You ought to glance at
Yahoo’s front page and see how they create article titles to grab viewers
to click. You might add a related video or a related pic or two to get readers excited about everything’ve written. Just my opinion, it could
make your website a little livelier.
I really love your blog.. Pleasant colors & theme.
Did you create this web site yourself? Please
reply back as I’m hoping to create my own personal site and would like to
find out where you got this from or exactly what the theme is
called. Thank you!
I couldn’t resist commenting. Very well written!
Informative article, exactly what I wanted to find.
Remarkable! Its in fact awesome article, I have got
much clear idea regarding from this paragraph.
With havin so much content and articles do you ever run into any issues of plagorism or copyright infringement?
My website has a lot of completely unique content I’ve either created myself or outsourced but it seems a lot of
it is popping it up all over the web without my agreement.
Do you know any ways to help reduce content from being stolen? I’d really appreciate it.
Wow! Finally I got a webpage from where I know how to genuinely obtain useful data concerning my study and knowledge.
A motivating discussion is worth comment. There’s no doubt that that you should write more on this
topic, it may not be a taboo subject but generally people don’t discuss these subjects.
To the next! All the best!!
Fantastic beat ! I wish to apprentice whilst you amend your website, how could
i subscribe for a blog site? The account helped me a appropriate deal.
I were tiny bit familiar of this your broadcast provided brilliant transparent concept
I really like what you guys are up too. This type of clever work and coverage!
Keep up the excellent works guys I’ve you
guys to my blogroll.
Hey There. I discovered your weblog the use of msn. This is a
really well written article. I will be sure to bookmark
it and return to read more of your useful info. Thanks for the post.
I’ll certainly comeback.
Hello to all, the contents existing at this website are in fact remarkable for people knowledge, well, keep up the nice
work fellows.
It’s not my first time to visit this web site, i am
browsing this web page dailly and take nice facts from
here all the time.
Hi, constantly i used to check website posts here in the
early hours in the break of day, for the reason that i like to
find out more and more.
It is perfect time to make a few plans for the long run and it is time to be happy.
I’ve learn this submit and if I could I want to counsel you few interesting issues
or suggestions. Maybe you can write next articles referring to this article.
I wish to read even more things approximately it!
Hello my friend! I wish to say that this post is amazing, nice written and come
with almost all significant infos. I would like to see more posts like this .
What a stuff of un-ambiguity and preserveness of valuable
familiarity concerning unpredicted emotions.
Hello! I could have sworn I’ve been to this website before but after checking through some of the post I realized it’s new to me.
Anyhow, I’m definitely glad I found it and I’ll be bookmarking and checking
back often!
It’s very trouble-free to find out any topic on net as compared to textbooks, as I found
this post at this web page.
We absolutely love your blog and find the majority of your post’s to
be what precisely I’m looking for. Does one offer guest
writers to write content in your case? I wouldn’t
mind publishing a post or elaborating on some of the
subjects you write about here. Again, awesome website!
constantly i used to read smaller posts which as well clear their motive, and that is also happening with this post which I am reading at
this time.
May I simply just say what a relief to discover an individual who truly understands what they are talking about on the internet.
You definitely realize how to bring a problem
to light and make it important. More people should look at this
and understand this side of the story. I was surprised you aren’t more popular
given that you surely have the gift.
Aw, this was an extremely good post. Taking the time and actual effort to make a great article… but what can I say… I procrastinate
a lot and don’t manage to get nearly anything
done.
Outstanding post however I was wanting to know if you could write a
litte more on this subject? I’d be very
grateful if you could elaborate a little bit
further. Many thanks!
I used to be able to find good advice from your blog articles.
Do you have a spam issue on this website; I also am a blogger, and I was wondering your situation;
we have created some nice methods and we are
looking to exchange methods with other folks,
please shoot me an email if interested.
Fantastic beat ! I would like to apprentice while you amend your web site,
how could i subscribe for a blog website? The account aided
me a acceptable deal. I had been tiny bit acquainted of this your broadcast offered bright
clear concept
Howdy just wanted to give you a quick heads up. The words
in your article seem to be running off the screen in Opera.
I’m not sure if this is a format issue or something
to do with web browser compatibility but I thought I’d post to
let you know. The design and style look great though!
Hope you get the issue fixed soon. Many thanks
Howdy! Do you use Twitter? I’d like to follow you
if that would be okay. I’m undoubtedly enjoying your blog and look forward
to new updates.
Woah! I’m really digging the template/theme of this site.
It’s simple, yet effective. A lot of times it’s very difficult to get that “perfect balance” between superb
usability and visual appeal. I must say you’ve done a amazing job with this.
Additionally, the blog loads extremely quick for me on Opera.
Exceptional Blog!
Hi colleagues, its wonderful post on the topic of tutoringand fully defined, keep it up
all the time.
Quality posts is the main to interest the users to visit the web page, that’s what this web page is providing.
Heya i’m for the primary time here. I came across this board and I find It really helpful & it helped me out
a lot. I hope to present one thing again and help others
like you helped me.
Unquestionably believe that which you said.
Your favorite reason seemed to be on the internet the
simplest thing to be aware of. I say to you,
I definitely get irked while people think about worries that they plainly do not know about.
You managed to hit the nail upon the top and also defined out the whole thing without having side effect
, people could take a signal. Will likely be back to get more.
Thanks
First off I would like to say fantastic blog! I had a quick question in which I’d like to ask if you
do not mind. I was interested to know how you center yourself and clear your head prior to writing.
I’ve had difficulty clearing my thoughts in getting my ideas out.
I do enjoy writing but it just seems like the first 10 to 15 minutes are wasted
just trying to figure out how to begin. Any ideas or tips?
Thank you!
Everything is very open with a clear explanation of
the challenges. It was really informative. Your
site is very useful. Thanks for sharing!
I absolutely love your blog and find many of your post’s to be just what I’m looking for.
Do you offer guest writers to write content in your case?
I wouldn’t mind creating a post or elaborating on a number of the subjects you write regarding here.
Again, awesome blog!
I visited various sites however the audio quality for audio songs current at
this website is really superb.
Thanks for sharing your thoughts about gocrot ip address.
Regards
You can certainly see your skills within the work
you write. The world hopes for even more passionate writers like you who aren’t afraid to say how
they believe. All the time follow your heart.
This article is truly a good one it helps new net users,
who are wishing for blogging.
Hey I am so glad I found your site, I really found you by error, while I was
browsing on Bing for something else, Nonetheless I am here
now and would just like to say thank you for a fantastic post and
a all round exciting blog (I also love the theme/design), I don’t have
time to go through it all at the minute but I have book-marked it and also added your RSS feeds, so when I have time I will be back to read a great deal
more, Please do keep up the awesome work.
Hey there! I know this is kinda off topic but I was wondering which blog platform are you using for this site?
I’m getting sick and tired of WordPress because I’ve had issues with hackers and I’m looking at options for another
platform. I would be fantastic if you could point
me in the direction of a good platform.
Greetings from Florida! I’m bored to tears at work so
I decided to browse your blog on my iphone during lunch break.
I really like the knowledge you present here and can’t wait to take a
look when I get home. I’m shocked at how quick your blog loaded on my
mobile .. I’m not even using WIFI, just 3G ..
Anyways, good blog!
Hi, its good piece of writing about media print, we all be aware of
media is a wonderful source of facts.
Hello it’s me, I am also visiting this website
daily, this site is actually good and the users are actually sharing good thoughts.
Amazing! This blog looks just like my old one! It’s on a completely different topic but it has pretty much the same page layout and design. Wonderful choice of colors!
Hi, I do believe this is a great blog. I stumbledupon it 😉 I will
return yet again since i have saved as a favorite it.
Money and freedom is the greatest way to change, may you be rich and
continue to guide others.
I could not resist commenting. Perfectly written!
Wow, awesome weblog layout! How long have you been running a blog for?
you made running a blog look easy. The entire glance
of your web site is wonderful, let alone the content material!
As the admin of this web page is working, no question very soon it will be famous,
due to its quality contents.
Amazing! This blog looks exactly like my old one! It’s on a totally different topic but it has pretty much the same page
layout and design. Outstanding choice of colors!
Every weekend i used to visit this web page, because i wish for enjoyment,
as this this web site conations genuinely good funny material too.
Yesterday, while I was at work, my cousin stole my apple ipad and tested
to see if it can survive a twenty five foot drop, just
so she can be a youtube sensation. My apple ipad is now destroyed and
she has 83 views. I know this is entirely off topic but I had to
share it with someone!
Greetings! I know this is kinda off topic but I was wondering if you knew where I could get a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having difficulty finding one?
Thanks a lot!
Hi there! Do you know if they make any plugins to help with Search Engine Optimization? I’m
trying to get my blog to rank for some targeted keywords but I’m not seeing
very good success. If you know of any please share.
Kudos!
I blog often and I genuinely appreciate your information. This article has really peaked my
interest. I am going to bookmark your blog and keep checking for
new details about once per week. I opted in for your Feed too.
Have you ever considered creating an e-book or guest authoring on other websites?
I have a blog centered on the same subjects you discuss and would really like to have you
share some stories/information. I know my viewers would
enjoy your work. If you’re even remotely interested, feel free to send me an email.
I’ve read several good stuff here. Definitely worth bookmarking for revisiting.
I surprise how much effort you place to create the sort of great informative site.
Hi to all, how is everything, I think every one is getting more from this web site,
and your views are nice in favor of new visitors.
Thanks for the marvelous posting! I actually enjoyed reading
it, you will be a great author.I will always bookmark your blog and will often come back later
in life. I want to encourage one to continue your
great posts, have a nice holiday weekend!
Fine way of explaining, and fastidious paragraph to take information on the topic of my presentation subject, which i am going to present in institution of
higher education.
I’m now not positive the place you’re getting your info, however great
topic. I must spend a while studying more or understanding more.
Thank you for wonderful information I was searching for this information for my mission.
There is certainly a lot to know about this topic. I love
all the points you have made.
My programmer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type
on several websites for about a year and am anxious about switching to another platform.
I have heard fantastic things about blogengine.net.
Is there a way I can transfer all my wordpress content into it?
Any help would be greatly appreciated!
I was curious if you ever thought of changing the page layout of your website?
Its very well written; I love what youve got to say. But maybe you could
a little more in the way of content so people could connect
with it better. Youve got an awful lot of text for only having one or two pictures.
Maybe you could space it out better?
Outstanding story there. What occurred after? Good luck!
I used to be able to find good information from your content.
I read this piece of writing completely on the
topic of the comparison of hottest and preceding technologies,
it’s amazing article.
Hi mates, its wonderful post regarding educationand completely defined, keep it up all the time.
Hello very cool site!! Man .. Beautiful .. Superb ..
I’ll bookmark your site and take the feeds additionally? I am satisfied to
find numerous helpful info here in the post, we want work out extra strategies in this regard, thanks for sharing.
. . . . .
Every weekend i used to visit this website, because i wish for enjoyment, for the
reason that this this web page conations truly nice funny stuff too.
If some one wants expert view on the topic of blogging and site-building then i advise him/her to pay
a visit this website, Keep up the fastidious job.
Your way of explaining the whole thing in this paragraph is really nice, all be capable
of simply understand it, Thanks a lot.
You are so interesting! I do not believe I’ve read a single thing like that before.
So wonderful to find someone with unique thoughts on this topic.
Really.. many thanks for starting this up.
This site is something that is needed on the internet,
someone with some originality!
Wow, superb blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your web site
is fantastic, let alone the content!
Sweet blog! I found it while surfing around on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo
News? I’ve been trying for a while but I never seem
to get there! Thanks
What’s Going down i am new to this, I stumbled
upon this I have discovered It absolutely helpful and it has aided
me out loads. I hope to contribute & aid other customers like its aided me.
Great job.
Do you have a spam problem on this website; I
also am a blogger, and I was wanting to know your situation; many of us have developed some nice practices and
we are looking to exchange techniques with other folks, please shoot me
an email if interested.
I all the time emailed this webpage post page to
all my contacts, since if like to read it afterward my
contacts will too.
Hello! I just wanted to ask if you ever have any trouble with hackers?
My last blog (wordpress) was hacked and I ended up losing months of
hard work due to no back up. Do you have any solutions to prevent hackers?
Hi there, I enjoy reading all of your article post. I wanted to write a little comment to support you.
What’s Happening i’m new to this, I stumbled upon this I’ve discovered It absolutely useful and it has aided
me out loads. I’m hoping to contribute & help other customers like its aided me.
Great job.
Hi, Neat post. There’s a problem with your website in internet
explorer, may check this? IE nonetheless is the marketplace leader and a big portion of other folks will pass
over your fantastic writing due to this problem.
It’s a pity you don’t have a donate button! I’d without a doubt donate
to this outstanding blog! I guess for now i’ll settle for book-marking and adding your RSS feed
to my Google account. I look forward to new updates and will talk about this site with my Facebook group.
Talk soon!
Hmm it appears like your site ate my first comment (it was super long) so I guess I’ll just sum it up
what I had written and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog writer but I’m still new to the whole thing.
Do you have any tips for newbie blog writers? I’d certainly appreciate it.
Thanks on your marvelous posting! I truly enjoyed reading it, you happen to be a great author.
I will be sure to bookmark your blog and will often come back at some point.
I want to encourage that you continue your great posts, have a nice afternoon!
You really make it seem so easy with your presentation but I find this
matter to be really something that I think I would never understand.
It seems too complicated and very broad for me.
I am looking forward for your next post, I will try to get the hang of it!
I’m excited to find this site. I wanted to thank you for
ones time due to this wonderful read!! I definitely loved
every little bit of it and i also have you book marked to look at new things in your site.
My spouse and I stumbled over here coming from a different website and thought I may as well check things out.
I like what I see so now i’m following you. Look forward
to exploring your web page for a second time.
Hey I know this is off topic but I was wondering if you knew of any widgets I could add
to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was
hoping maybe you would have some experience with something like this.
Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to
your new updates.
Wow, amazing weblog format! How long have you ever been running a blog for?
you make blogging look easy. The entire glance of your web site is great, let alone the content material!
I love looking through a post that can make people think.
Also, thanks for permitting me to comment!
It is perfect time to make some plans for the future
and it’s time to be happy. I have read this post and if I could I want to
suggest you few interesting things or suggestions. Perhaps
you can write next articles referring to this article.
I wish to read more things about it!
Useful info. Fortunate me I found your website by accident, and I’m surprised why
this accident didn’t happened in advance!
I bookmarked it.
Unquestionably consider that which you stated. Your favorite justification appeared to be at the net the easiest factor to have in mind of.
I say to you, I certainly get annoyed even as other people think about concerns that they just do not
know about. You controlled to hit the nail upon the highest as smartly as defined
out the entire thing without having side-effects , people can take a signal.
Will likely be again to get more. Thanks
Hello there! Quick question that’s totally off topic. Do
you know how to make your site mobile friendly? My site looks weird when browsing from my iphone.
I’m trying to find a theme or plugin that might be able to correct this
issue. If you have any recommendations, please share.
Cheers!
Pretty! This has been an extremely wonderful post.
Many thanks for supplying this information.
Very nice article, just what I needed.
Amazing issues here. I’m very glad to see your article. Thank you so much
and I’m having a look forward to contact you. Will you kindly drop me a mail?
Hi there all, here every one is sharing these familiarity, thus it’s
nice to read this weblog, and I used to go to see this webpage daily.
Hi, i believe that i saw you visited my blog so i came to go back the choose?.I am attempting to to find
issues to improve my site!I guess its adequate to make use of
some of your concepts!!
My partner and I stumbled over here coming from a different web
address and thought I might as well check things out.
I like what I see so now i’m following you.
Look forward to checking out your web page again.
I’m truly enjoying the design and layout of your blog.
It’s a very easy on the eyes which makes it much more
pleasant for me to come here and visit more often. Did you hire out a designer to
create your theme? Excellent work!
Yesterday, while I was at work, my sister stole my iphone and tested
to see if it can survive a 40 foot drop, just so she can be a youtube sensation. My apple ipad is now destroyed and she has 83 views.
I know this is completely off topic but I had to share it with someone!
Thank you for sharing your info. I truly appreciate your efforts and I will be waiting for your next write ups thanks
once again.
I’m really enjoying the theme/design of your weblog.
Do you ever run into any browser compatibility
issues? A number of my blog readers have complained about my blog not operating correctly in Explorer but looks
great in Firefox. Do you have any solutions to help fix this issue?
Excellent goods from you, man. I’ve understand your stuff
previous to and you’re just too excellent. I actually like what you have acquired
here, really like what you are stating and the
way in which you say it. You make it enjoyable and
you still care for to keep it smart. I can’t wait to read much more from you.
This is really a tremendous web site.
My brother suggested I might like this blog. He was entirely right.
This post truly made my day. You can not imagine just how much time I had spent
for this info! Thanks!
You can definitely see your enthusiasm within the work you write.
The sector hopes for more passionate writers like you who
are not afraid to say how they believe. All the
time go after your heart.
Thanks for your marvelous posting! I actually enjoyed reading
it, you are a great author.I will make sure to bookmark your blog and may come back very soon. I
want to encourage you continue your great writing, have a nice
weekend!
No matter if some one searches for his vital thing, so he/she
wants to be available that in detail, thus that thing is
maintained over here.
Pretty component to content. I simply stumbled upon your website and in accession capital to assert that I
acquire in fact loved account your blog posts.
Any way I’ll be subscribing for your augment and even I
achievement you access consistently quickly.
Thanks for sharing such a pleasant thought, article is nice, thats why i have read it entirely
I would like to thank you for the efforts you’ve put in penning this site.
I am hoping to view the same high-grade content from you in the future as
well. In truth, your creative writing abilities has inspired me to get my own, personal site now 😉
This info is worth everyone’s attention. How can I find out
more?
That is very fascinating, You are an overly skilled blogger.
I’ve joined your rss feed and sit up for in quest of extra
of your magnificent post. Additionally, I have
shared your website in my social networks
I was wondering if you ever considered changing the layout of your site?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could
connect with it better. Youve got an awful lot of text for only having 1 or two pictures.
Maybe you could space it out better?
It’s the best time to make a few plans for the long run and it is time to be
happy. I’ve read this put up and if I may I wish to recommend you some fascinating things or
suggestions. Maybe you can write next articles regarding this
article. I want to learn more things about it!
I enjoy what you guys are usually up too. Such clever work and
exposure! Keep up the superb works guys I’ve incorporated
you guys to my blogroll.
I’m really loving the theme/design of your site.
Do you ever run into any browser compatibility problems? A small
number of my blog audience have complained about my blog not working correctly in Explorer but looks great in Safari.
Do you have any tips to help fix this problem?
If you are going for finest contents like I do, simply visit this
website all the time for the reason that it gives
quality contents, thanks
Heya i am for the first time here. I came across this board and
I to find It truly helpful & it helped me out much.
I am hoping to present one thing back and aid others like you helped me.
I like the valuable information you provide for your articles.
I will bookmark your weblog and take a look at once more here regularly.
I’m rather sure I’ll learn plenty of new stuff
proper right here! Best of luck for the following!
It’s really a cool and helpful piece of info. I am happy that you simply shared this useful
info with us. Please keep us informed like this.
Thank you for sharing.
Every weekend i used to pay a visit this website, because i
want enjoyment, since this this site conations in fact nice funny material too.
Thanks , I have just been looking for info approximately this subject for ages and yours is the greatest I’ve discovered
so far. However, what in regards to the bottom line?
Are you sure in regards to the source?
I am truly grateful to the holder of this web page who
has shared this fantastic article at at this time.
Today, I went to the beach with my children. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She
put the shell to her ear and screamed. There was a hermit crab inside
and it pinched her ear. She never wants to go back!
LoL I know this is completely off topic but I had to tell someone!
I blog often and I really appreciate your content. This article has really peaked my interest.
I will bookmark your site and keep checking for new details about once
per week. I opted in for your Feed as well.
It’s actually a cool and useful piece of information. I am satisfied that you shared
this helpful info with us. Please keep us informed like this.
Thank you for sharing.
I visited several sites however the audio feature
for audio songs current at this site is genuinely excellent.
you’re in reality a good webmaster. The web site loading pace is incredible.
It seems that you’re doing any distinctive trick.
Moreover, The contents are masterwork. you’ve done a great process in this
matter!
I blog often and I truly thank you for your
information. The article has really peaked my interest.
I’m going to take a note of your website and keep checking for new information about once a week.
I opted in for your Feed as well.
Good post however , I was wanting to know if
you could write a litte more on this subject? I’d be very thankful if you could elaborate a little bit further.
Bless you!
I am really thankful to the owner of this web page who has shared this great post at at this
time.
Thanks for any other informative web site. The place else may I am getting
that type of information written in such an ideal manner?
I’ve a challenge that I am just now running on, and I’ve been on the
look out for such information.
Good post. I learn something totally new and challenging on websites I stumbleupon everyday.
It will always be exciting to read content from other authors and practice
a little something from other sites.
I am in fact thankful to the holder of this web site who has shared this wonderful post at here.
Thanks to my father who shared with me regarding this weblog,
this weblog is actually remarkable.
Hello there! This is my 1st comment here so I just wanted to give a quick shout out and tell you I really enjoy reading through your blog posts.
Can you suggest any other blogs/websites/forums that go over the same subjects?
Appreciate it!
Awesome site you have here but I was wanting
to know if you knew of any discussion boards that cover the same topics talked about in this article?
I’d really like to be a part of online community where I can get advice from other knowledgeable people that share
the same interest. If you have any recommendations, please
let me know. Kudos!
It’s difficult to find knowledgeable people
on this subject, but you seem like you know what you’re talking about!
Thanks
My brother recommended I might like this blog. He was entirely right.
This post truly made my day. You cann’t imagine just how much time I had
spent for this information! Thanks!
Thanks designed for sharing such a good thinking,
post is fastidious, thats why i have read it completely
I have been browsing online more than three hours today, but I by no means
discovered any attention-grabbing article like yours. It is beautiful
price sufficient for me. Personally, if all web owners
and bloggers made good content material as you probably did, the internet might be a lot more useful than ever before.
Whoa! This blog looks just like my old one! It’s on a totally
different subject but it has pretty much the same page layout and design. Great choice of colors!
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get three e-mails
with the same comment. Is there any way you can remove me
from that service? Cheers!
Excellent post. I was checking continuously this weblog and I’m inspired!
Very useful info specially the last part 🙂 I handle such information much.
I used to be looking for this certain information for
a very long time. Thanks and best of luck.
Good answers in return of this query with solid arguments and explaining the whole thing regarding that.
If you desire to take much from this article then you have to apply these techniques to
your won web site.
Hmm it seems like your site ate my first comment (it was extremely long) so I guess I’ll just sum it up
what I wrote and say, I’m thoroughly enjoying your blog. I too am an aspiring blog writer but
I’m still new to everything. Do you have any helpful hints for newbie blog writers?
I’d certainly appreciate it.
Greetings, There’s no doubt that your site may
be having web browser compatibility issues. When I look at your blog in Safari, it looks fine however when opening in IE,
it’s got some overlapping issues. I just wanted to provide you with a quick heads up!
Apart from that, excellent site!
What’s up, yup this article is in fact pleasant
and I have learned lot of things from it concerning blogging.
thanks.
My partner and I stumbled over here different web page and
thought I might check things out. I like what I see so now i am
following you. Look forward to checking out your web page again.
Just want to say your article is as astonishing. The clarity in your put up is just
great and i could suppose you’re an expert on this subject.
Well with your permission let me to grasp your feed to stay updated with approaching post.
Thank you one million and please continue
the rewarding work.
You can definitely see your expertise within the article you write.
The arena hopes for more passionate writers such as you who are not afraid to say how they believe.
All the time go after your heart.
I used to be able to find good information from
your articles.
Wow, this article is pleasant, my sister is analyzing these kinds of things,
therefore I am going to convey her.
I’m truly enjoying the design and layout of your website.
It’s a very easy on the eyes which makes it much more enjoyable for me to come here
and visit more often. Did you hire out a developer to create your theme?
Superb work!
Nice post. I was checking continuously this blog and I am impressed!
Very useful information specially the last part 🙂 I care for such information a lot.
I was looking for this particular information for a
long time. Thank you and good luck.
Hey there I am so excited I found your webpage, I really found you by error, while
I was searching on Digg for something else, Anyways I am here now and
would just like to say kudos for a fantastic post
and a all round entertaining blog (I also love the theme/design),
I don’t have time to browse it all at the moment but I have book-marked it and also added your RSS feeds, so when I have time
I will be back to read a lot more, Please do keep up the superb work.
I loved as much as you will receive carried
out right here. The sketch is attractive, your authored material stylish.
nonetheless, you command get bought an impatience over that you wish be
delivering the following. unwell unquestionably come more formerly again as exactly the same nearly a lot
often inside case you shield this increase.
Great beat ! I wish to apprentice while you amend your site,
how could i subscribe for a blog web site? The account helped me a
acceptable deal. I had been a little bit acquainted of this your broadcast offered bright
clear concept
Hi there! Someone in my Myspace group shared this site with us so I
came to check it out. I’m definitely enjoying the information. I’m bookmarking and
will be tweeting this to my followers! Wonderful blog and fantastic style
and design.
Awesome article.
I enjoy what you guys are up too. Such clever work and reporting!
Keep up the good works guys I’ve added you guys to blogroll.
Howdy, i read your blog from time to time and i own a similar
one and i was just curious if you get a lot of spam comments?
If so how do you protect against it, any plugin or anything
you can suggest? I get so much lately it’s driving me crazy
so any support is very much appreciated.
Definitely believe that which you stated. Your favorite justification seemed to be on the net the simplest thing to be aware of.
I say to you, I definitely get annoyed while people think about worries that they plainly do not know about.
You managed to hit the nail upon the top and also defined out the whole thing without having side-effects ,
people can take a signal. Will likely be back to
get more. Thanks
Definitely believe that which you stated. Your favorite reason appeared to be
on the internet the simplest thing to be aware of. I say to you, I definitely get annoyed while people think
about worries that they plainly don’t know about. You managed to
hit the nail upon the top as well as defined out the whole thing without having side effect , people could take
a signal. Will probably be back to get more. Thanks
Hi there, all is going fine here and ofcourse every one is sharing
facts, that’s genuinely good, keep up writing.
Wow, that’s what I was exploring for, what a data!
present here at this webpage, thanks admin of this web page.
My partner and I stumbled over here by a different page and thought I may
as well check things out. I like what I see
so i am just following you. Look forward to looking into your web page yet again.
You really make it seem so easy with your presentation but I find this matter to be actually
something which I think I would never understand. It seems too complex and very broad for me.
I’m looking forward for your next post, I’ll try to get the hang
of it!
With havin so much written content do you ever run into any problems of plagorism
or copyright infringement? My site has a lot of exclusive content I’ve either written myself or outsourced but it seems a lot of
it is popping it up all over the web without my permission. Do you know any methods to help reduce content from being ripped off?
I’d certainly appreciate it.
Hi everyone, it’s my first go to see at this web site, and article
is actually fruitful in favor of me, keep up posting these types of articles.
I know this if off topic but I’m looking into starting my own blog and was wondering what all is required to get set up?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very web savvy so I’m not 100% positive. Any recommendations or advice would be greatly
appreciated. Appreciate it
Simply desire to say your article is as astonishing. The clearness in your publish is simply spectacular and
i can assume you’re a professional on this subject. Well together with
your permission let me to seize your feed to keep up to date
with forthcoming post. Thank you 1,000,000 and please continue the gratifying work.
It’s remarkable to go to see this web page and reading the views of all mates about this paragraph,
while I am also keen of getting knowledge.
Hi there, I enjoy reading through your article.
I like to write a little comment to support you.
hello!,I like your writing so much! proportion we keep in touch
extra about your article on AOL? I require a specialist in this area to resolve my problem.
May be that is you! Having a look ahead to see you.
Superb blog you have here but I was wanting to know if you knew of any message boards that cover the same topics
discussed in this article? I’d really like to be a part of group
where I can get feedback from other knowledgeable people that share the same interest.
If you have any recommendations, please let me know.
Thanks a lot!
Somebody necessarily help to make significantly articles I’d state.
This is the very first time I frequented your website page and so far?
I amazed with the analysis you made to make this actual submit extraordinary.
Magnificent job!
I absolutely love your website.. Excellent colors & theme.
Did you develop this web site yourself? Please reply back as I’m looking to create my very own site and would love to find out
where you got this from or what the theme is called. Thanks!
Very descriptive article, I liked that bit. Will there be a part
2?
Excellent blog you’ve got here.. It’s hard to find excellent writing like yours these days.
I truly appreciate individuals like you! Take care!!
My developer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type on several websites for about a year and am anxious about switching to another platform.
I have heard excellent things about blogengine.net. Is there a way I can transfer all my
wordpress posts into it? Any help would be really appreciated!
I loved as much as you will receive carried out right here.
The sketch is tasteful, your authored material stylish. nonetheless,
you command get got an impatience over that you wish be delivering the following.
unwell unquestionably come more formerly again since
exactly the same nearly very often inside case you shield
this hike.
If some one wants expert view concerning blogging after that i propose him/her to pay a
quick visit this web site, Keep up the nice job.
First off I want to say excellent blog! I had a quick question in which I’d
like to ask if you do not mind. I was curious to know
how you center yourself and clear your mind prior to writing.
I have had a tough time clearing my mind in getting my
thoughts out. I do enjoy writing however it just seems like the first 10 to 15 minutes tend
to be wasted simply just trying to figure out how to
begin. Any suggestions or tips? Kudos!
You are so awesome! I don’t believe I have read anything like that before.
So great to discover another person with a few genuine thoughts
on this issue. Really.. thank you for starting this up.
This website is something that is needed on the web,
someone with some originality!
If some one wants expert view regarding blogging after that i
recommend him/her to pay a quick visit this blog, Keep up the fastidious work.
Good day I am so thrilled I found your webpage, I really found you
by error, while I was researching on Yahoo for something else, Anyhow
I am here now and would just like to say thanks for a tremendous post
and a all round thrilling blog (I also love the theme/design), I don’t have time to browse it all at the moment
but I have bookmarked it and also included your RSS feeds,
so when I have time I will be back to read a lot more, Please do keep up the great job.
With havin so much content and articles do you ever run into any problems of plagorism
or copyright infringement? My site has a lot of unique content I’ve either authored myself or outsourced but it looks like a lot of it is popping it up all over
the internet without my authorization. Do you know any ways to help reduce
content from being stolen? I’d truly appreciate it.
Thanks for every other great post. Where else may anybody get
that type of info in such a perfect method of writing?
I’ve a presentation subsequent week, and I’m at the search for such information.
Hey great blog! Does running a blog similar to this require a lot of work?
I have absolutely no expertise in coding however I was hoping to start my
own blog in the near future. Anyways, if you have any recommendations or techniques for new
blog owners please share. I know this is off topic nevertheless I just had to ask.
Appreciate it!
Sweet blog! I found it while surfing around on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Many thanks
Hey there! Would you mind if I share your blog with my
facebook group? There’s a lot of people that I think would really enjoy your content.
Please let me know. Thank you
Thanks for one’s marvelous posting! I certainly enjoyed
reading it, you’re a great author.I will be sure to bookmark
your blog and definitely will come back sometime soon. I want to encourage you to ultimately
continue your great job, have a nice day!
Hmm it seems like your site ate my first
comment (it was super long) so I guess I’ll just sum it up what I wrote and
say, I’m thoroughly enjoying your blog. I too am an aspiring blog blogger but I’m still new to everything.
Do you have any tips for first-time blog writers? I’d definitely appreciate it.
You could definitely see your expertise within the work you write.
The world hopes for more passionate writers like you who are not afraid to mention how they
believe. All the time go after your heart.
Hi there everyone, it’s my first visit at this web site,
and piece of writing is genuinely fruitful in favor of me,
keep up posting such articles or reviews.
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I get actually enjoyed account your blog posts.
Anyway I’ll be subscribing to your augment and even I achievement you access consistently rapidly.
Very great post. I simply stumbled upon your blog and wanted to mention that
I have truly loved browsing your weblog posts.
In any case I will be subscribing in your
rss feed and I’m hoping you write once more soon!
Hi there, just wanted to say, I liked this blog post. It was inspiring.
Keep on posting!
Hello, i think that i saw you visited my web site thus i came to “return the favor”.I am trying to find things to
enhance my web site!I suppose its ok to
use some of your ideas!!
Spot on with this write-up, I actually believe that this site needs far more attention. I’ll probably
be back again to see more, thanks for the advice!
Hi there, after reading this amazing piece of writing i am as well delighted to share my experience here
with colleagues.
Great post however , I was wanting to know if you could write a litte
more on this subject? I’d be very thankful if you could elaborate a little bit more.
Kudos!
You could definitely see your enthusiasm within the article you write.
The arena hopes for more passionate writers such as you who
are not afraid to say how they believe. All the time go after your heart.
It is not my first time to pay a visit this web page, i am visiting this web page dailly and get fastidious data from here everyday.
First off I would like to say excellent blog! I had a quick question that I’d like
to ask if you do not mind. I was interested to find out how you center yourself and clear your mind prior to writing.
I have had trouble clearing my mind in getting my ideas out.
I truly do take pleasure in writing however it just seems like the first 10 to 15 minutes are generally wasted simply just trying to figure out how to begin. Any suggestions or hints?
Kudos!
If you are going for finest contents like myself, only pay a visit this web site everyday for the reason that it presents
quality contents, thanks
Asking questions are genuinely pleasant thing if you are not understanding anything entirely, but this post presents pleasant
understanding yet.
We’re a bunch of volunteers and opening a new scheme in our community.
Your web site provided us with helpful info to work on. You have done an impressive activity and our whole community
might be thankful to you.
Hi, I desire to subscribe for this blog to take
newest updates, so where can i do it please assist.
Hi, all the time i used to check web site posts here
early in the morning, for the reason that i like to gain knowledge of more
and more.
you’re actually a just right webmaster. The web site loading
velocity is amazing. It kind of feels that you are doing any distinctive trick.
In addition, The contents are masterpiece. you’ve done a excellent process on this matter!
I am not sure where you are getting your info, but good topic.
I must spend some time studying much more or figuring out more.
Thank you for magnificent information I was in search of this information for my
mission.
Thanks for your marvelous posting! I seriously enjoyed reading it, you may be a great author.
I will be sure to bookmark your blog and may come back down the road.
I want to encourage you to ultimately continue your great writing, have
a nice holiday weekend!
Do you have a spam issue on this site; I also am a blogger, and I was wanting to know your
situation; we have developed some nice procedures and we are
looking to trade solutions with other folks, please shoot me an e-mail if
interested.
I have been surfing online more than 2 hours today, yet I never found any interesting
article like yours. It is pretty worth enough for me.
Personally, if all website owners and bloggers made good content as you did, the internet will
be a lot more useful than ever before.
It’s very simple to find out any topic on net as compared to books,
as I found this post at this site.
It’s very straightforward to find out any topic on net as compared to
textbooks, as I found this post at this web page.
Spot on with this write-up, I honestly feel this site needs a great deal more attention.
I’ll probably be returning to read more, thanks for the information!
You actually make it seem really easy with your presentation however I to find this
matter to be really something which I think I’d never understand.
It kind of feels too complicated and very broad for me.
I’m having a look forward for your subsequent submit,
I’ll attempt to get the dangle of it!
Heya are using WordPress for your site platform? I’m new to the
blog world but I’m trying to get started and create my own. Do you require any html coding knowledge to make your own blog?
Any help would be really appreciated!
For newest news you have to go to see web and on world-wide-web I found
this web page as a best website for most up-to-date updates.
Hello there! This is kind of off topic but I need some
help from an established blog. Is it very hard to set up
your own blog? I’m not very techincal but I can figure things out pretty fast.
I’m thinking about making my own but I’m not sure where to
begin. Do you have any ideas or suggestions? Cheers
I think the admin of this website is truly working hard for his web site, since here
every data is quality based data.
I enjoy what you guys tend to be up too. This type of clever work and reporting!
Keep up the fantastic works guys I’ve incorporated you
guys to my blogroll.
Pretty nice post. I simply stumbled upon your weblog and wished to say that I’ve truly loved surfing around your blog
posts. In any case I will be subscribing in your feed and I’m hoping you write once more soon!
What’s Happening i am new to this, I stumbled upon this
I’ve discovered It absolutely helpful and it has aided me
out loads. I’m hoping to give a contribution & aid different customers like its aided me.
Good job.
I think what you published made a bunch of sense.
But, what about this? what if you were to create a killer post title?
I am not suggesting your information isn’t good., however what if you added
a post title that makes people want more? I mean Adhesive Capsulitis: A Sticky Issue – Agile Ortho is kinda boring.
You should look at Yahoo’s home page and note how they write post titles to grab viewers to open the
links. You might add a related video or a picture
or two to grab readers excited about what you’ve written. Just my
opinion, it would make your posts a little livelier.
It’s enormous that you are getting thoughts from this
paragraph as well as from our discussion made at this place.
Hi there, i read your blog occasionally and i own a similar one and
i was just curious if you get a lot of spam feedback?
If so how do you stop it, any plugin or anything you can suggest?
I get so much lately it’s driving me crazy so any support is
very much appreciated.
Sweet blog! I found it while browsing on Yahoo News. Do
you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there!
Cheers
Can you tell us more about this? I’d care to find out some additional information.
Yes! Finally someone writes about lendir abg.
Because the admin of this site is working, no hesitation very quickly it will
be famous, due to its quality contents.
Hello it’s me, I am also visiting this web site regularly, this site is in fact fastidious
and the visitors are really sharing good thoughts.
I visited many blogs however the audio feature for audio songs current at this site is truly marvelous.
I know this website provides quality based articles and
other stuff, is there any other website which
gives such data in quality?
At this time it seems like BlogEngine is the preferred blogging platform out there right now.
(from what I’ve read) Is that what you’re using on your
blog?
Greetings from Los angeles! I’m bored to death at work so I decided to browse your
site on my iphone during lunch break. I really like the
info you provide here and can’t wait to take a look
when I get home. I’m amazed at how fast your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyhow, very good blog!
Please let me know if you’re looking for a article author for your
weblog. You have some really great posts and I feel I would be a good asset.
If you ever want to take some of the load off, I’d really like to write some articles for
your blog in exchange for a link back to mine. Please send me an e-mail if interested.
Cheers!
Have you ever considered writing an ebook or guest
authoring on other blogs? I have a blog based upon on the same topics you discuss and would really like to have you share some stories/information. I know my visitors would
appreciate your work. If you are even remotely interested, feel free to send me an e mail.
Hmm it appears like your site ate my first comment (it was super long) so I
guess I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog blogger but I’m still new to everything.
Do you have any tips for beginner blog writers? I’d definitely appreciate it.
Peculiar article, exactly what I was looking for.
Hi there all, here every person is sharing such knowledge, thus it’s pleasant
to read this website, and I used to go to see this webpage every day.
Excellent way of describing, and good paragraph to get information about my presentation subject, which i am going
to convey in academy.
Saved as a favorite, I like your website!
I’ve been browsing online more than 4 hours today, yet
I never found any interesting article like yours. It’s pretty worth enough for me.
Personally, if all web owners and bloggers made good
content as you did, the net will be a lot more useful than ever before.
Great post however , I was wanting to know if you could write
a litte more on this subject? I’d be very grateful if you could elaborate a little bit further.
Appreciate it!
I really like your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you?
Plz answer back as I’m looking to create
my own blog and would like to find out where u got
this from. many thanks
I always used to read piece of writing in news papers
but now as I am a user of net therefore from now I
am using net for articles, thanks to web.
Every weekend i used to go to see this web site,
as i want enjoyment, since this this site conations
actually pleasant funny material too.
I’ve been surfing online greater than three hours lately, but
I never discovered any interesting article like yours.
It is beautiful worth enough for me. Personally, if all website owners and bloggers made
just right content as you did, the net might be a lot more helpful than ever before.
Good answer back in return of this difficulty with
genuine arguments and describing everything on the topic of that.
If you are going for finest contents like myself, simply pay
a visit this web site daily for the reason that it offers quality contents,
thanks
It’s wonderful that you are getting thoughts from this piece of writing as
well as from our dialogue made at this place.
It’s remarkable to go to see this web site and reading the views of all mates concerning this paragraph, while
I am also eager of getting know-how.
I always used to study piece of writing in news papers but
now as I am a user of web so from now I am using net for articles, thanks to web.
Just want to say your article is as astounding. The clearness to your submit is just excellent
and that i can think you are an expert on this subject.
Well with your permission let me to take hold of your feed to stay up to date with forthcoming post.
Thank you 1,000,000 and please carry on the gratifying work.
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now
each time a comment is added I get three e-mails with
the same comment. Is there any way you can remove people from that service?
Appreciate it!
Yes! Finally someone writes about yupoo.
Hi there, just wanted to say, I liked this blog post. It was funny.
Keep on posting!
Hi there! I know this is kind of off topic but I was wondering which blog platform
are you using for this site? I’m getting tired of WordPress because I’ve had
problems with hackers and I’m looking at alternatives for another platform.
I would be great if you could point me in the direction of a good platform.
Hey There. I found your blog using msn. This is a very well written article.
I’ll be sure to bookmark it and return to read more of your useful info.
Thanks for the post. I will definitely comeback.
It’s awesome designed for me to have a web site, which is helpful
in favor of my knowledge. thanks admin
Hello, its nice piece of writing concerning media print, we
all be familiar with media is a enormous source of data.
Greetings! Very helpful advice within this post!
It is the little changes that will make the most significant changes.
Thanks a lot for sharing!
This is a topic which is near to my heart…
Many thanks! Where are your contact details though?
Hello to every body, it’s my first go to see of this blog; this
webpage contains awesome and really fine material for readers.
Tremendous things here. I am very satisfied
to see your post. Thank you a lot and I’m looking forward to touch you.
Will you kindly drop me a mail?
An interesting discussion is worth comment. I believe that you should publish more
about this topic, it may not be a taboo subject but usually
people don’t talk about such topics. To the next!
All the best!!
Usually I do not learn article on blogs, but
I wish to say that this write-up very forced me to try and
do it! Your writing style has been amazed me. Thanks, quite great article.
Hello, i feel that i saw you visited my website so i got here to go back the prefer?.I am trying to
to find things to improve my web site!I suppose its ok to use a few of your
ideas!!
This post is really a good one it helps new internet viewers, who
are wishing for blogging.
What’s up everyone, it’s my first pay a visit at this web site,
and post is truly fruitful in favor of me, keep up posting such articles.
Hello there! This is my first comment here so I just wanted to
give a quick shout out and tell you I truly enjoy reading through your articles.
Can you recommend any other blogs/websites/forums that deal with the same topics?
Thanks for your time!
I’m amazed, I must say. Rarely do I encounter a blog that’s equally educative and amusing, and let me tell you, you have hit
the nail on the head. The issue is something not enough
men and women are speaking intelligently about. I’m very happy that I stumbled
across this during my search for something regarding this.
An impressive share! I have just forwarded this onto a friend who had been doing a little homework on this.
And he in fact ordered me dinner simply because I found it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanx for spending time to talk about this matter
here on your web page.
This is a great tip particularly to those fresh to the blogosphere.
Short but very precise information… Thanks for sharing this one.
A must read article!
That is very fascinating, You’re an excessively professional blogger.
I have joined your feed and look ahead to in the hunt for more of your excellent post.
Additionally, I have shared your site in my social networks
Fabulous, what a web site it is! This weblog provides useful information to
us, keep it up.
This is very interesting, You’re a very skilled blogger.
I’ve joined your rss feed and look forward to seeking more of your fantastic post.
Also, I have shared your site in my social networks!
It is perfect time to make some plans for the long run and
it’s time to be happy. I have read this submit and if I may I desire to counsel you some interesting
things or advice. Perhaps you could write next articles referring to this article.
I wish to read more issues approximately it!
Just want to say your article is as astounding.
The clarity to your submit is simply spectacular and
that i can suppose you’re a professional on this subject.
Fine along with your permission allow me to take hold of your feed to keep up to date with impending post.
Thanks 1,000,000 and please continue the rewarding work.
Remarkable issues here. I’m very glad to see your article.
Thanks a lot and I am having a look forward to contact you.
Will you kindly drop me a mail?
Good day! I know this is somewhat off topic but I was wondering
if you knew where I could find a captcha plugin for
my comment form? I’m using the same blog platform as
yours and I’m having trouble finding one? Thanks a
lot!
What’s up, I read your blogs on a regular basis.
Your story-telling style is awesome, keep up the good work!
Have you ever considered writing an e-book or guest authoring on other sites?
I have a blog based on the same ideas you discuss and would love to
have you share some stories/information. I know my audience
would value your work. If you are even remotely interested, feel free to shoot me an email.
Everything is very open with a very clear explanation of
the issues. It was truly informative. Your website is extremely helpful.
Thanks for sharing!
Unquestionably believe that which you said. Your favorite reason appeared to
be on the internet the simplest thing to be aware of.
I say to you, I definitely get irked while people think about worries that
they just do not know about. You managed to hit the nail upon the top and also defined out the whole thing without having
side effect , people could take a signal. Will probably
be back to get more. Thanks
It’s in fact very complicated in this full of activity
life to listen news on Television, therefore I
just use world wide web for that reason, and obtain the hottest information.
hi!,I really like your writing very a lot! proportion we communicate extra about your article on AOL?
I require an expert on this house to resolve my problem.
May be that is you! Taking a look ahead to peer you.
My programmer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type
on a variety of websites for about a year and am concerned about switching to another platform.
I have heard fantastic things about blogengine.net. Is there a
way I can import all my wordpress content into it?
Any kind of help would be greatly appreciated!
My partner and I stumbled over here from a different page and
thought I might check things out. I like what I see so i am just following you.
Look forward to looking over your web page yet again.
I’m amazed, I must say. Seldom do I encounter a blog that’s both educative and
engaging, and without a doubt, you have hit the nail on the head.
The problem is something not enough men and women are speaking intelligently about.
I am very happy I found this in my search for something regarding this.
Fantastic goods from you, man. I have understand your stuff previous to and you’re
just too wonderful. I actually like what you have acquired here, certainly like what you
are stating and the way in which you say it. You make it entertaining and you still care for to keep it wise.
I can’t wait to read far more from you. This
is really a tremendous web site.
Wow! Finally I got a web site from where I know how
to in fact take helpful data regarding my study and knowledge.
This paragraph will help the internet viewers for creating new blog
or even a blog from start to end.
I couldn’t refrain from commenting. Perfectly written!
Hi there! Someone in my Myspace group shared this website with us so I came
to give it a look. I’m definitely enjoying the information. I’m bookmarking and will be tweeting this to my followers!
Outstanding blog and superb design and style.
Fastidious replies in return of this issue with real arguments and explaining the whole thing
about that.
Today, while I was at work, my sister stole my apple ipad and tested to
see if it can survive a forty foot drop, just so she can be
a youtube sensation. My iPad is now broken and she has 83 views.
I know this is completely off topic but I had to share it with someone!
I do trust all the ideas you have offered to your post. They are really convincing and can certainly
work. Nonetheless, the posts are too quick for novices.
May you please extend them a bit from subsequent time?
Thanks for the post.
It is truly a great and helpful piece of information. I am glad that you simply shared this useful information with us.
Please keep us informed like this. Thanks for sharing.
Thank you for any other fantastic article. Where else
may anyone get that kind of information in such an ideal
manner of writing? I have a presentation subsequent week, and I
am on the search for such information.
I always emailed this weblog post page to all my contacts, as if like to
read it then my contacts will too.
I’m extremely impressed with your writing skills and also with the layout on your weblog.
Is this a paid theme or did you modify it yourself?
Anyway keep up the nice quality writing, it’s rare to see a great blog like this one nowadays.
You could definitely see your expertise within the work you write.
The sector hopes for even more passionate writers like you who are
not afraid to mention how they believe. Always follow your heart.
Pretty! This was an incredibly wonderful post.
Thanks for supplying this information.
What a data of un-ambiguity and preserveness of precious know-how about unpredicted feelings.
Hey I know this is off topic but I was wondering if you knew of any widgets I could add
to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time
and was hoping maybe you would have some experience with
something like this. Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your new updates.
I seriously love your blog.. Very nice colors & theme. Did you build this site yourself?
Please reply back as I’m looking to create my own personal site and want to learn where you got this
from or just what the theme is called. Thanks!
I’m extremely impressed along with your writing skills and
also with the layout for your blog. Is this a paid theme
or did you customize it your self? Either way keep up the excellent quality writing, it is rare to peer a nice weblog like this one these days..
I’m impressed, I must say. Rarely do I come across
a blog that’s equally educative and amusing,
and without a doubt, you have hit the nail on the head.
The problem is something that not enough folks are speaking intelligently about.
Now i’m very happy I stumbled across this during my hunt
for something concerning this.
Thank you, I have recently been looking for info about
this topic for a long time and yours is the best I’ve came upon so far.
But, what in regards to the conclusion? Are you sure in regards
to the supply?
What’s Happening i’m new to this, I stumbled upon this I’ve discovered
It positively useful and it has helped me out loads. I’m hoping
to contribute & help other users like its aided me.
Great job.
Do you have any video of that? I’d love to find out some additional information.
Thank you a bunch for sharing this with all people you actually recognise what you’re talking about!
Bookmarked. Please additionally consult with my web
site =). We will have a hyperlink alternate contract between us
Great post. I was checking continuously this weblog and I am inspired!
Extremely helpful info specially the last
section 🙂 I maintain such information a lot. I used to be
seeking this certain information for a very lengthy time.
Thank you and best of luck.
This paragraph offers clear idea in favor of the new people of blogging, that truly how to do blogging and site-building.
This text is priceless. How can I find out more?
Greetings! Very useful advice within this post! It is the little changes which will make
the most significant changes. Thanks for sharing!
I love what you guys are usually up too. Such clever work and
coverage! Keep up the fantastic works guys I’ve included you
guys to blogroll.
Cool blog! Is your theme custom made or did
you download it from somewhere? A design like yours with a few simple
adjustements would really make my blog jump out.
Please let me know where you got your design. Kudos
Post writing is also a excitement, if you be acquainted
with then you can write or else it is complex to write.
Hello, i think that i saw you visited my website thus i came to “return the favor”.I am trying to
find things to improve my web site!I suppose its
ok to use a few of your ideas!!
Good day very cool web site!! Man .. Excellent ..
Wonderful .. I will bookmark your website and take the feeds also?
I’m happy to seek out a lot of helpful information here within the put up, we need work
out more strategies on this regard, thank you
for sharing. . . . . .
Hi there Dear, are you actually visiting this web page on a regular basis,
if so after that you will definitely take nice experience.
Simply want to say your article is as amazing. The clarity in your post is just
nice and i could assume you are an expert on this subject.
Fine with your permission let me to grab your RSS feed to keep updated with forthcoming post.
Thanks a million and please continue the gratifying work.
Thanks for the auspicious writeup. It in reality was a
amusement account it. Look advanced to far introduced agreeable
from you! By the way, how could we be in contact?
Thanks designed for sharing such a good idea, post is nice,
thats why i have read it fully
I’ve been exploring for a bit for any high quality articles or blog
posts on this sort of house . Exploring in Yahoo I ultimately stumbled upon this website.
Reading this information So i’m happy to convey that
I’ve an incredibly excellent uncanny feeling I found out exactly what
I needed. I most unquestionably will make sure to don?t put out of your mind this
site and give it a glance regularly.
This article presents clear idea in favor of the new
people of blogging, that truly how to do blogging and site-building.
Hey there would you mind sharing which blog platform you’re working with?
I’m looking to start my own blog in the near future but I’m having a hard time making a decision between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design and style seems different
then most blogs and I’m looking for something
completely unique. P.S Apologies for getting off-topic but
I had to ask!
Quality articles is the secret to attract the people
to pay a quick visit the web site, that’s what this site is providing.
Highly descriptive blog, I liked that a lot. Will there be a part 2?
Great site you’ve got here.. It’s hard to find high quality writing like yours these days.
I truly appreciate people like you! Take care!!
Great blog here! Also your site loads up fast!
What host are you using? Can I get your affiliate link to your host?
I wish my web site loaded up as quickly as yours lol
I am no longer positive the place you are getting your information, but great topic.
I must spend some time learning much more or figuring out more.
Thanks for excellent info I was looking for this information for
my mission.
You made some decent points there. I looked on the web to learn more about the
issue and found most people will go along with your views on this website.
Hi there! I just wanted to ask if you ever have any issues with hackers?
My last blog (wordpress) was hacked and I ended up losing several
weeks of hard work due to no backup. Do you
have any solutions to prevent hackers?
Can I simply just say what a comfort to find someone who truly understands what they’re discussing online.
You definitely know how to bring an issue
to light and make it important. A lot more
people ought to check this out and understand this side of the story.
I was surprised you aren’t more popular given that you surely possess the gift.
At this moment I am going to do my breakfast, later than having
my breakfast coming over again to read further news.
Hello this is somewhat of off topic but I was wanting to know
if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding knowledge so I wanted to get
guidance from someone with experience. Any help would be greatly
appreciated!
Your style is really unique in comparison to other folks I’ve
read stuff from. Many thanks for posting when you’ve got the opportunity, Guess
I’ll just book mark this page.
Hi! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any tips?
Post writing is also a excitement, if you be familiar with after that you can write if not it is difficult to write.
Thank you for another informative website. Where
else may I am getting that type of info written in such an ideal manner?
I’ve a venture that I am simply now running on, and I’ve been at the
glance out for such information.
I pay a visit every day some blogs and blogs to
read content, but this weblog offers feature based
articles.
Hey there would you mind sharing which blog platform you’re using?
I’m looking to start my own blog soon but I’m having a difficult time deciding between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design seems different then most blogs
and I’m looking for something unique.
P.S Apologies for being off-topic but I had to ask!
Sweet blog! I found it while searching on Yahoo News.
Do you have any suggestions on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Thank you
wonderful publish, very informative. I wonder why the other
experts of this sector don’t notice this. You must continue your writing.
I am confident, you have a huge readers’ base already!
Wow, this article is nice, my sister is analyzing these
things, thus I am going to tell her.
My brother recommended I might like this
website. He used to be entirely right. This publish actually made my day.
You can not consider just how so much time
I had spent for this info! Thank you!
It’s actually a cool and helpful piece of info. I am satisfied that you simply shared
this useful info with us. Please stay us informed like this.
Thanks for sharing.
Generally I do not read post on blogs, but I would like to
say that this write-up very forced me to try and do
so! Your writing style has been surprised me. Thank you, quite great post.
We’re a group of volunteers and opening a new scheme in our community.
Your web site provided us with valuable information to work on. You
have done an impressive job and our entire community will be thankful to you.
Incredible! This blog looks just like my old one! It’s on a completely different topic but
it has pretty much the same layout and design. Great choice of colors!
Excellent beat ! I wish to apprentice while you amend your site, how could i subscribe for
a blog web site? The account aided me a acceptable deal.
I had been tiny bit acquainted of this your broadcast provided bright clear idea
Hmm it looks like your website ate my first comment (it was
super long) so I guess I’ll just sum it up what I had written and say, I’m thoroughly enjoying your blog.
I as well am an aspiring blog blogger but I’m still new to the whole thing.
Do you have any recommendations for inexperienced blog writers?
I’d really appreciate it.
Definitely imagine that that you stated. Your favorite reason appeared to be at the internet
the easiest factor to be aware of. I say to you, I definitely get annoyed whilst other folks consider worries that they just do not recognize about.
You managed to hit the nail upon the top and also outlined out
the whole thing with no need side effect , people can take a signal.
Will likely be back to get more. Thanks
I really like it when people get together and share thoughts.
Great site, stick with it!
I have to thank you for the efforts you’ve put in penning
this blog. I really hope to see the same high-grade content by you in the future as well.
In fact, your creative writing abilities has inspired me to
get my own, personal blog now 😉
I want to to thank you for this fantastic read!!
I absolutely enjoyed every little bit of it. I’ve got you bookmarked to check out new stuff you
post…
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment
is added I get several emails with the same comment.
Is there any way you can remove people from that service?
Bless you!
There is definately a great deal to know about this topic.
I really like all the points you’ve made.
Undeniably believe that which you stated. Your favorite justification seemed to be on the web the simplest thing
to be aware of. I say to you, I certainly get irked while people consider worries that they just don’t know about.
You managed to hit the nail upon the top as well as defined out the whole thing without having side effect ,
people can take a signal. Will likely be back to get
more. Thanks
Hey there! I’ve been following your website for a while now and finally got the
bravery to go ahead and give you a shout out from
Huffman Tx! Just wanted to say keep up the fantastic
job!
You really make it seem so easy with your presentation but I find
this matter to be actually something which I think I would never understand.
It seems too complex and very broad for me. I am looking forward for your next post, I will try to get the hang of
it!
Oh my goodness! Awesome article dude! Thank you, However
I am encountering difficulties with your RSS. I don’t understand why I cannot join it.
Is there anybody getting similar RSS issues? Anybody who knows the answer will you
kindly respond? Thanx!!
It’s appropriate time to make a few plans for the longer term and it’s time to be happy.
I’ve learn this post and if I may just I want to counsel you some attention-grabbing
things or suggestions. Maybe you can write next articles regarding this article.
I desire to read more issues approximately it!
Thanks in favor of sharing such a good thinking, article is pleasant, thats why i have read it completely
I think the admin of this website is really working hard in favor of
his site, since here every information is quality based
data.
Woah! I’m really loving the template/theme of this blog.
It’s simple, yet effective. A lot of times it’s challenging to
get that “perfect balance” between usability and visual appearance.
I must say you’ve done a awesome job with this. Also, the blog loads very fast for me on Chrome.
Exceptional Blog!
I think this is among the most vital information for
me. And i am glad reading your article. But should remark on some general things,
The website style is ideal, the articles is really nice :
D. Good job, cheers
Attractive component to content. I simply stumbled upon your web site and in accession capital to
assert that I acquire actually enjoyed account your weblog posts.
Anyway I will be subscribing for your augment and even I
success you access consistently fast.
What a material of un-ambiguity and preserveness of precious
familiarity regarding unpredicted feelings.
I think the admin of this web page is actually working hard in favor of his web
site, as here every material is quality based material.
Hi, I want to subscribe for this weblog to take most up-to-date updates, so where can i do it please help
out.
I’m amazed, I have to admit. Seldom do I come across a blog that’s both educative and amusing,
and without a doubt, you have hit the nail on the head.
The problem is something not enough people are speaking
intelligently about. Now i’m very happy that I found this in my hunt
for something concerning this.
Hey! Do you use Twitter? I’d like to follow
you if that would be okay. I’m definitely enjoying
your blog and look forward to new posts.
A fascinating discussion is definitely worth comment.
I believe that you ought to publish more about this subject matter, it might not be a taboo matter but usually people don’t talk about such issues.
To the next! All the best!!
Do you have a spam problem on this website; I also am a blogger,
and I was wondering your situation; many of us have developed some nice
methods and we are looking to trade techniques with other
folks, why not shoot me an email if interested.
I know this web page presents quality depending articles or reviews and additional data,
is there any other web page which gives these kinds
of data in quality?
I’m not sure where you’re getting your info, but good topic.
I needs to spend some time learning more or understanding more.
Thanks for wonderful info I was looking for this information for my mission.
If you desire to obtain a great deal from this post then you have to apply
such techniques to your won weblog.
Its like you read my thoughts! You appear to grasp so
much approximately this, such as you wrote the e
book in it or something. I think that you just can do
with some percent to power the message home a bit, however other than that, that is magnificent blog.
An excellent read. I’ll certainly be back.
Howdy! I know this is kinda off topic but I was wondering if you knew
where I could locate a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having trouble finding one?
Thanks a lot!
bookmarked!!, I like your web site!
Thanks for every other informative blog. Where else may just
I am getting that kind of information written in such a perfect method?
I’ve a mission that I am just now running on, and I’ve been at the look out for such info.
Hi! I’ve been reading your blog for a while now and finally got the bravery to
go ahead and give you a shout out from Humble Texas! Just wanted
to tell you keep up the excellent work!
Hello there! This blog post couldn’t be written much better!
Going through this post reminds me of my previous roommate!
He always kept talking about this. I will send this article to him.
Fairly certain he’s going to have a good read. Thanks for sharing!
Hi, everything is going nicely here and ofcourse every one is sharing data, that’s
truly excellent, keep up writing.
Whoa! This blog looks exactly like my old one! It’s on a entirely different subject but it has pretty much the
same layout and design. Great choice of colors!
Fantastic web site. Plenty of helpful information here.
I’m sending it to several pals ans also sharing in delicious.
And certainly, thanks on your effort!
You actually make it seem so easy with your presentation but I
find this matter to be really something that I
think I would never understand. It seems too complex and
very broad for me. I’m looking forward for your next post, I’ll
try to get the hang of it!
I have read so many articles or reviews regarding the blogger lovers but this post
is actually a good paragraph, keep it up.
Excellent post! We will be linking to this particularly great article
on our site. Keep up the great writing.
I was curious if you ever thought of changing the page layout of your website?
Its very well written; I love what youve got to say. But maybe you could a little more in the way of
content so people could connect with it better.
Youve got an awful lot of text for only having 1 or 2 pictures.
Maybe you could space it out better?
What a stuff of un-ambiguity and preserveness of precious familiarity concerning unexpected feelings.
Does your website have a contact page? I’m having problems locating it but, I’d like to send you an email.
I’ve got some recommendations for your blog you might be interested in hearing.
Either way, great website and I look forward to seeing it improve over time.
My spouse and I stumbled over here from a different website and thought I should check things out.
I like what I see so i am just following you.
Look forward to checking out your web page again.
Thank you for any other great post. Where else may just
anybody get that type of info in such an ideal means of writing?
I’ve a presentation next week, and I am on the search for such information.
Thanks a bunch for sharing this with all people you really realize what you are
speaking approximately! Bookmarked. Please additionally discuss with my site =).
We can have a hyperlink alternate contract among us
Thank you for the good writeup. It in fact was a amusement account it.
Look advanced to far added agreeable from you! However, how can we communicate?
I’ve been surfing online more than three hours today, yet I never found
any interesting article like yours. It’s pretty worth enough for me.
Personally, if all site owners and bloggers made good
content as you did, the web will be much more
useful than ever before.
An impressive share! I’ve just forwarded this onto a co-worker who was doing a little research on this.
And he actually bought me breakfast due to the fact that I discovered it
for him… lol. So allow me to reword this…. Thanks for the meal!!
But yeah, thanx for spending some time to discuss this subject here on your site.
There is certainly a great deal to learn about this subject.
I like all the points you’ve made.
I was excited to find this page. I want to to thank you for your time just for this
wonderful read!! I definitely really liked every bit of
it and i also have you saved to fav to see new information in your web site.
Hi there all, here every one is sharing these experience, thus it’s
good to read this weblog, and I used to pay a quick
visit this webpage all the time.
Hey There. I found your blog using msn. This is a really well written article.
I’ll make sure to bookmark it and come back to read more of your useful information.
Thanks for the post. I will certainly return.
May I just say what a comfort to discover somebody that truly understands what
they are discussing online. You certainly understand how to bring
an issue to light and make it important. More and more people have to
read this and understand this side of your story.
I was surprised that you’re not more popular since you most certainly possess the gift.
Greetings from Los angeles! I’m bored to death at work so
I decided to check out your site on my iphone
during lunch break. I enjoy the information you present here and can’t wait to take a look when I get home.
I’m shocked at how fast your blog loaded on my mobile ..
I’m not even using WIFI, just 3G .. Anyhow, amazing blog!
We are a gaggle of volunteers and starting a new scheme in our community.
Your site offered us with useful information to work on. You’ve done a formidable job and our entire community will
likely be thankful to you.
It’s amazing to pay a quick visit this website and reading the
views of all mates regarding this piece of writing, while
I am also zealous of getting experience.
Hi, always i used to check webpage posts here early in the break of day,
as i love to find out more and more.
Just desire to say your article is as surprising. The clearness in your post is simply spectacular and i could assume you’re an expert on this subject.
Fine with your permission let me to grab your RSS feed to keep updated with
forthcoming post. Thanks a million and please continue
the gratifying work.
Wonderful blog! I found it while surfing around on Yahoo
News. Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Thanks
Magnificent site. Plenty of useful information here.
I am sending it to several pals ans also sharing in delicious.
And certainly, thanks in your sweat!
Wonderful article! This is the kind of info that should be shared around the net.
Disgrace on the seek engines for no longer positioning this post
higher! Come on over and discuss with my
website . Thank you =)
Excellent post. I used to be checking constantly
this weblog and I am inspired! Extremely useful info particularly the ultimate
part 🙂 I deal with such information much.
I used to be seeking this certain information for a very long time.
Thanks and good luck.
It’s going to be ending of mine day, except before ending
I am reading this impressive piece of writing to improve my
know-how.
This post is worth everyone’s attention. How can I find out more?
Sweet blog! I found it while searching on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Thank you
Appreciating the dedication you put into your site and detailed information you present.
It’s good to come across a blog every once in a while that isn’t the same unwanted rehashed
material. Excellent read! I’ve bookmarked your site and I’m
including your RSS feeds to my Google account.
Now I am ready to do my breakfast, once having my breakfast coming
over again to read other news.
Do you have any video of that? I’d like to find out
some additional information.
Hello just wanted to give you a quick heads up. The words in your
post seem to be running off the screen in Chrome. I’m not sure if this is a formatting issue or something to
do with internet browser compatibility but I thought I’d post to let you know.
The design and style look great though! Hope you get the problem solved
soon. Thanks
Hi! This post could not be written any better! Reading this post reminds me of my good old room
mate! He always kept chatting about this. I will forward this page to him.
Fairly certain he will have a good read. Thanks for sharing!
Everyone loves it when people get together and share ideas.
Great blog, continue the good work!
I do accept as true with all the concepts you have presented on your post.
They are really convincing and can definitely work.
Still, the posts are very short for novices. Could you please extend them
a little from subsequent time? Thanks for the post.
constantly i used to read smaller articles that also clear their
motive, and that is also happening with this article which I am reading
now.
I visited various websites except the audio feature for audio songs existing
at this website is in fact wonderful.
I am regular reader, how are you everybody? This piece of
writing posted at this website is in fact good.
Hello everyone, it’s my first go to see at this web page, and paragraph is genuinely fruitful
designed for me, keep up posting such content.
I like the helpful information you supply on your articles.
I’ll bookmark your weblog and test once more here frequently.
I am relatively sure I’ll be told plenty of new stuff right right here!
Best of luck for the following!
First of all I want to say superb blog! I had a quick question in which I’d like to ask if you don’t mind.
I was interested to find out how you center yourself and clear your head prior
to writing. I have had trouble clearing my mind in getting my thoughts out.
I do enjoy writing but it just seems like the first 10 to 15
minutes are generally lost just trying to figure out how to begin. Any
recommendations or hints? Thanks!
This article will assist the internet users for building up new blog or
even a blog from start to end.
It is the best time to make a few plans for the future and it is time
to be happy. I’ve learn this put up and if I may I wish to
counsel you some fascinating issues or suggestions.
Maybe you could write next articles referring to this article.
I desire to learn even more issues approximately it!
Hi outstanding website! Does running a blog like this require a large amount of work?
I’ve very little expertise in programming but I had been hoping to start my own blog soon. Anyway, if you have
any recommendations or techniques for new blog owners please share.
I understand this is off topic but I just needed to ask.
Thank you!
Pretty! This was a really wonderful post. Thanks for providing these details.
Normally I do not learn article on blogs, but I would
like to say that this write-up very compelled me to take a
look at and do it! Your writing style has been surprised me.
Thank you, very great article.
Valuable information. Fortunate me I found your site
unintentionally, and I’m shocked why this twist of fate didn’t came about earlier!
I bookmarked it.
I have read so many articles or reviews on the topic of the blogger lovers except this paragraph is actually a
fastidious piece of writing, keep it up.
I visited various blogs except the audio feature for audio songs present at this web site is really wonderful.
My relatives always say that I am killing my time here at net, but I know I am getting
familiarity everyday by reading such pleasant articles or
reviews.
Hey There. I found your blog using msn. This is a very well written article.
I will be sure to bookmark it and return to read more of your useful info.
Thanks for the post. I will certainly return.
This is really attention-grabbing, You’re a very professional blogger.
I have joined your rss feed and stay up for looking for
extra of your wonderful post. Also, I’ve shared your website in my social networks
Everyone loves what you guys tend to be up too.
Such clever work and reporting! Keep up the good works guys I’ve added you guys to my
personal blogroll.
It’s genuinely very difficult in this full of activity life to listen news on TV, therefore I just use internet for that purpose, and obtain the newest news.
I was recommended this blog by my cousin. I’m not sure whether this post is written by him as no one else know such detailed about my trouble.
You’re wonderful! Thanks!
Oh my goodness! Amazing article dude! Thanks, However I am having issues with your
RSS. I don’t know the reason why I am unable to subscribe
to it. Is there anybody having similar RSS issues?
Anyone that knows the answer will you kindly respond?
Thanx!!
Hello there! Quick question that’s completely off topic.
Do you know how to make your site mobile friendly?
My web site looks weird when viewing from my iphone4. I’m trying to find a theme or plugin that might be able to fix this
issue. If you have any recommendations, please share. Thank you!
I like what you guys tend to be up too. This kind of clever work and coverage!
Keep up the good works guys I’ve included you guys to my personal blogroll.
When I initially commented I clicked the “Notify me when new comments are added” checkbox and now each time a
comment is added I get four emails with the same comment.
Is there any way you can remove people from that service?
Cheers!
Howdy! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying
to get my blog to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Appreciate it!
This is really interesting, You are a very skilled blogger.
I’ve joined your rss feed and look forward to seeking more
of your fantastic post. Also, I’ve shared your site in my social networks!
Write more, thats all I have to say. Literally, it seems as though you relied on the video to
make your point. You definitely know what youre talking about,
why throw away your intelligence on just posting
videos to your weblog when you could be giving us something informative to read?
Wonderful blog! I found it while searching on Yahoo News.
Do you have any tips on how to get listed in Yahoo
News? I’ve been trying for a while but I never seem to get there!
Thanks
This text is worth everyone’s attention. How can I find out
more?
Hello there! This post could not be written any better!
Reading through this post reminds me of my previous room mate!
He always kept talking about this. I will forward this page to him.
Fairly certain he will have a good read. Many thanks
for sharing!
Howdy! I know this is somewhat off topic but I was wondering which
blog platform are you using for this website?
I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at options for another
platform. I would be awesome if you could point me in the direction of a good platform.
With havin so much content do you ever run into any issues of plagorism or copyright violation?
My blog has a lot of completely unique content I’ve
either written myself or outsourced but it seems a lot of it is popping
it up all over the web without my agreement. Do you know any techniques
to help protect against content from being ripped off?
I’d genuinely appreciate it.
What i don’t realize is if truth be told how you’re not really a
lot more smartly-appreciated than you may be now.
You are very intelligent. You understand therefore
significantly on the subject of this topic, produced me for my part consider it from so many
various angles. Its like men and women aren’t interested unless it is one thing to do with Lady gaga!
Your individual stuffs outstanding. At all times take care of it
up!
naturally like your web site but you need to test the spelling on quite a few of your posts.
Several of them are rife with spelling problems and I to find it very bothersome to inform
the reality then again I’ll certainly come again again.
Awesome issues here. I am very glad to peer your article.
Thanks so much and I am having a look ahead to touch you.
Will you please drop me a e-mail?
I blog quite often and I seriously appreciate your information. This article has truly
peaked my interest. I will bookmark your site and keep checking for new information about once
a week. I subscribed to your RSS feed as well.
I blog often and I genuinely appreciate your information. Your article has truly peaked my interest.
I will bookmark your site and keep checking for new information about once a week.
I opted in for your RSS feed too.
Do you have any video of that? I’d want to find out more details.
You really make it seem really easy together with your presentation but I
to find this topic to be actually one thing that I think I might never understand.
It seems too complex and very extensive for me.
I am having a look ahead on your next post, I’ll try to get the cling of it!
At this time it seems like Expression Engine is the best
blogging platform out there right now. (from what I’ve read) Is that what you’re using on your blog?
My developer is trying to convince me to move
to .net from PHP. I have always disliked the idea because
of the expenses. But he’s tryiong none the less. I’ve been using Movable-type on a number of
websites for about a year and am worried about switching to another platform.
I have heard excellent things about blogengine.net. Is there a way I can transfer all my wordpress content into it?
Any help would be really appreciated!
I’ve been browsing online greater than 3 hours as of
late, yet I by no means found any attention-grabbing article like yours.
It is lovely value sufficient for me. In my view, if all website owners and bloggers made good content material as
you did, the web will likely be a lot more useful than ever before.
Hi there, the whole thing is going perfectly here
and ofcourse every one is sharing information, that’s in fact
excellent, keep up writing.
Wow, fantastic blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your web site is magnificent, let alone the content!
If you are going for finest contents like myself, simply visit this site all the time because
it gives quality contents, thanks
After checking out a handful of the articles on your website,
I seriously like your technique of blogging.
I saved as a favorite it to my bookmark webpage
list and will be checking back soon. Take a look at my website too
and tell me what you think.
Spot on with this write-up, I really feel this site needs a lot more attention. I’ll probably be back again to see more, thanks for the information!
Just wish to say your article is as amazing. The
clearness in your post is just nice and i can assume you are an expert on this subject.
Well with your permission allow me to grab your feed to keep updated with forthcoming post.
Thanks a million and please continue the enjoyable work.
I loved as much as you’ll receive carried out
right here. The sketch is tasteful, your authored material stylish.
nonetheless, you command get got an nervousness over that you wish be delivering the
following. unwell unquestionably come more formerly again since exactly the same
nearly a lot often inside case you shield this hike.
Undeniably imagine that which you stated. Your favorite justification seemed to be on the internet the simplest factor to
take into account of. I say to you, I definitely get annoyed while people think about issues that they plainly don’t realize about.
You controlled to hit the nail upon the top and outlined out the entire thing without having
side-effects , folks can take a signal. Will probably be again to get
more. Thank you
Great article.
I take pleasure in, cause I found exactly what I was looking for.
You have ended my 4 day long hunt! God Bless you man. Have a great day.
Bye
Hi there, after reading this awesome article i am
also delighted to share my familiarity here with mates.
Hello to all, how is all, I think every one is getting more from this web
page, and your views are nice in support of new viewers.
I’m gone to say to my little brother, that he should
also visit this weblog on regular basis to obtain updated from newest gossip.
I’m amazed, I must say. Seldom do I come across a blog that’s equally educative and amusing, and let me tell you, you’ve hit the nail on the head.
The problem is an issue that not enough folks are speaking intelligently about.
I’m very happy I came across this in my hunt for something concerning this.
Hola! I’ve been reading your website for a while now and
finally got the courage to go ahead and give you a shout out from Kingwood Tx!
Just wanted to mention keep up the fantastic work!
I used to be able to find good info from your blog posts.
Hello it’s me, I am also visiting this site regularly, this site is in fact good and the visitors
are truly sharing good thoughts.
I am curious to find out what blog platform you are working with?
I’m experiencing some small security problems with my latest site and I would
like to find something more risk-free. Do you have any recommendations?
I always spent my half an hour to read this web site’s articles everyday along with a mug
of coffee.
Good day! Would you mind if I share your blog with
my twitter group? There’s a lot of people that I think would really appreciate your content.
Please let me know. Many thanks
This is a very good tip particularly to those fresh to the blogosphere.
Brief but very precise information… Appreciate your sharing this
one. A must read post!
Greetings! I’ve been reading your website for a while now and finally got
the bravery to go ahead and give you a shout out
from Porter Tx! Just wanted to mention keep up the great work!
Very rapidly this site will be famous among all blogging and site-building visitors, due to
it’s good content
I every time emailed this blog post page to all my associates, since if like to read it then my contacts will too.
Fantastic goods from you, man. I have understand your stuff previous to
and you are just extremely excellent. I really like what you have acquired here, really like what you are saying and the
way in which you say it. You make it entertaining and you still take care
of to keep it smart. I cant wait to read far more from you.
This is really a wonderful website.
If you are going for most excellent contents like me,
only go to see this web site all the time because it presents feature contents, thanks
It’s nearly impossible to find knowledgeable people in this particular subject,
but you sound like you know what you’re talking about!
Thanks
Have you ever considered about adding a little bit more
than just your articles? I mean, what you say is important and everything.
But think about if you added some great photos or video clips to give your posts more, “pop”!
Your content is excellent but with pics and clips, this blog could certainly be one of the most beneficial in its field.
Amazing blog!
There is certainly a great deal to know about this subject.
I really like all the points you’ve made.
I was suggested this web site by my cousin. I’m not sure whether this
post is written by him as no one else know such detailed about my difficulty.
You’re wonderful! Thanks!
Fantastic blog! Do you have any hints for aspiring writers?
I’m hoping to start my own website soon but I’m a little lost on everything.
Would you suggest starting with a free platform like WordPress
or go for a paid option? There are so many choices out there that I’m completely
overwhelmed .. Any ideas? Many thanks!
Way cool! Some extremely valid points! I appreciate
you writing this article and the rest of the site is also really good.
I am actually delighted to read this weblog
posts which carries plenty of useful data, thanks for providing these information.
Its not my first time to visit this site, i am visiting this web page dailly and take
pleasant facts from here everyday.
I blog frequently and I seriously thank you for your content.
The article has really peaked my interest.
I am going to take a note of your blog and keep checking for new information about once per
week. I opted in for your RSS feed too.
Today, I went to the beach front with my kids. I found a
sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put
the shell to her ear and screamed. There was a hermit
crab inside and it pinched her ear. She never wants to go
back! LoL I know this is completely off topic but I had to tell someone!
It’s remarkable in favor of me to have a website, which is useful in support of my knowledge.
thanks admin
Spot on with this write-up, I actually think
this web site needs a lot more attention. I’ll probably be back again to see
more, thanks for the info!
Asking questions are truly fastidious thing if you are not understanding something totally, except this piece of writing offers pleasant understanding
yet.
First of all I would like to say excellent blog!
I had a quick question in which I’d like to ask if you do not mind.
I was interested to know how you center yourself and clear
your head prior to writing. I have had a hard time clearing
my mind in getting my ideas out. I truly do take pleasure in writing
but it just seems like the first 10 to 15 minutes are wasted simply just trying
to figure out how to begin. Any recommendations or tips?
Many thanks!
Hi mates, how is the whole thing, and what you desire to say
concerning this post, in my view its genuinely amazing in support of me.
Hi there! I understand this is somewhat off-topic but I needed to ask.
Does building a well-established blog like yours require a massive amount work?
I am brand new to writing a blog but I do write in my diary everyday.
I’d like to start a blog so I can share my experience and views online.
Please let me know if you have any kind of suggestions
or tips for brand new aspiring blog owners. Thankyou!
Hi there to every body, it’s my first go to see of this weblog; this website
carries awesome and in fact good data in support of visitors.
This post offers clear idea for the new viewers of blogging, that really how to do blogging and site-building.
What’s Taking place i am new to this, I stumbled upon this
I’ve found It absolutely useful and it has helped me out
loads. I hope to give a contribution & aid different
users like its aided me. Great job.
This design is steller! You definitely know how to keep a reader amused.
Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Excellent job.
I really enjoyed what you had to say, and more than that,
how you presented it. Too cool!
Today, I went to the beach front with my children. I found a sea shell and
gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She
put the shell to her ear and screamed. There was a hermit crab
inside and it pinched her ear. She never wants to go back!
LoL I know this is entirely off topic but I had to tell someone!
Its such as you learn my mind! You seem to understand
a lot about this, such as you wrote the guide in it or
something. I feel that you just can do with some p.c.
to pressure the message house a little bit, but other than that, this is excellent blog.
A fantastic read. I’ll definitely be back.
Does your site have a contact page? I’m having problems
locating it but, I’d like to shoot you an email.
I’ve got some recommendations for your blog you might be interested
in hearing. Either way, great website and I look forward to seeing it grow
over time.
Wow, this paragraph is fastidious, my sister is analyzing these things, therefore I am going to
tell her.
Hi to all, how is the whole thing, I think every one is getting more
from this site, and your views are good for new visitors.
It’s very effortless to find out any topic on net as compared to books, as I found this paragraph at this site.
Good day! I could have sworn I’ve been to this site before
but after going through many of the articles I realized it’s new to me.
Anyhow, I’m definitely delighted I came across it and I’ll be book-marking it and checking back frequently!
Excellent post. I was checking continuously this blog and I am
inspired! Very helpful information specially the remaining section :
) I handle such info much. I used to be seeking this certain info for a long time.
Thank you and good luck.
Thanks for the auspicious writeup. It in truth was once a entertainment
account it. Glance complex to far introduced agreeable from
you! However, how could we communicate?
My coder is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using WordPress on various
websites for about a year and am nervous about switching to another platform.
I have heard excellent things about blogengine.net. Is there a way
I can import all my wordpress content into it?
Any kind of help would be really appreciated!
Hey! I just wanted to ask if you ever have any issues
with hackers? My last blog (wordpress) was hacked and I ended up losing many
months of hard work due to no backup. Do you have any methods to stop
hackers?
Hello there! I could have sworn I’ve been to this website before but after reading
through some of the post I realized it’s new to me. Anyways, I’m definitely delighted I found it and I’ll be bookmarking
and checking back often!
Spot on with this write-up, I seriously feel this amazing
site needs a great deal more attention. I’ll probably be returning to see more,
thanks for the advice!
Hi colleagues, how is all, and what you would like to say
on the topic of this paragraph, in my view its really amazing for me.
I visited multiple websites but the audio quality for
audio songs current at this web page is truly wonderful.
Good day! I just want to give you a huge thumbs up for your great info you have got here on this post.
I will be returning to your web site for more soon.
Fantastic site you have here but I was curious about
if you knew of any message boards that cover the same topics talked
about in this article? I’d really like to be a part of community where I can get
responses from other experienced people that
share the same interest. If you have any suggestions, please let me know.
Thanks a lot!
I am curious to find out what blog platform you are working with?
I’m having some small security problems with my latest
blog and I’d like to find something more safe. Do you
have any solutions?
Thank you for the good writeup. It in fact was a amusement account it.
Look advanced to far added agreeable from you! By the way, how can we communicate?
Wow! Finally I got a web site from where I can really take helpful information concerning my study and
knowledge.
I’ll immediately seize your rss as I can not find your e-mail subscription link or
e-newsletter service. Do you have any? Please allow me understand so that I may subscribe.
Thanks.
Very good post. I will be dealing with some of these issues as
well..
I’m really loving the theme/design of your web site.
Do you ever run into any internet browser compatibility issues?
A few of my blog audience have complained about my
website not working correctly in Explorer but looks great in Safari.
Do you have any ideas to help fix this issue?
I was curious if you ever thought of changing
the layout of your blog? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content
so people could connect with it better. Youve got an awful lot of text for only having one or 2 images.
Maybe you could space it out better?
When someone writes an post he/she maintains the plan of a user in his/her
mind that how a user can know it. Therefore that’s why this post is
outstdanding. Thanks!
First of all I want to say excellent blog!
I had a quick question that I’d like to ask if you don’t
mind. I was curious to find out how you center yourself and clear your head prior
to writing. I’ve had a tough time clearing my thoughts in getting my thoughts out.
I do take pleasure in writing but it just seems like the first 10 to 15 minutes tend to be wasted simply just trying to figure out
how to begin. Any recommendations or hints? Kudos!
When I initially left a comment I appear to have clicked on the -Notify me when new comments are
added- checkbox and now each time a comment is added I get 4 emails with
the same comment. Perhaps there is a way you are able to remove me from that service?
Cheers!
Unquestionably believe that that you said. Your favorite justification seemed to
be on the internet the easiest thing to be mindful of.
I say to you, I certainly get annoyed whilst people consider worries that they plainly do not know about.
You controlled to hit the nail upon the top and
defined out the entire thing without having side-effects , other folks can take
a signal. Will likely be again to get more. Thanks
I’ve been exploring for a bit for any high-quality articles or blog posts in this sort of area
. Exploring in Yahoo I at last stumbled upon this website.
Studying this info So i’m satisfied to convey that I’ve a very good uncanny feeling I discovered just what I needed.
I such a lot surely will make certain to don?t put out of your mind this site and give it a glance regularly.
I read this paragraph completely regarding the comparison of most recent and earlier technologies, it’s remarkable
article.
I for all time emailed this website post page to all my
friends, since if like to read it next my friends will too.
Undeniably believe that which you stated. Your favorite justification seemed to
be on the web the simplest thing to be aware of. I say to
you, I certainly get annoyed while people think about worries that they plainly don’t know about.
You managed to hit the nail upon the top and defined out the whole thing
without having side-effects , people can take a signal.
Will likely be back to get more. Thanks
That is a very good tip especially to those fresh to
the blogosphere. Simple but very precise info… Appreciate your sharing this one.
A must read article!
I’m gone to convey my little brother, that he should also go to see this weblog on regular basis
to get updated from hottest information.
I every time emailed this blog post page to all my friends, for the reason that if like to read it
then my contacts will too.
Thanks for sharing your info. I really appreciate your
efforts and I am waiting for your next write ups thank you once again.
I am not sure the place you are getting your info, but great topic.
I must spend some time finding out much more or figuring out more.
Thanks for magnificent information I used to be
on the lookout for this information for my mission.
Excellent blog here! Also your site loads up fast!
What host are you using? Can I get your affiliate link to your
host? I wish my web site loaded up as quickly as yours lol
Hello there! Quick question that’s totally off topic.
Do you know how to make your site mobile friendly?
My web site looks weird when browsing from my iphone 4. I’m trying to find
a template or plugin that might be able to fix this
problem. If you have any suggestions, please share. Thank you!
This is very interesting, You’re a very skilled blogger.
I’ve joined your rss feed and look forward to seeking more of your great post.
Also, I have shared your web site in my social networks!
Hi there, this weekend is fastidious in favor of me, since this point in time i am reading this
great educational article here at my house.
Nice post. I was checking constantly this blog and I’m inspired!
Extremely helpful info particularly the closing phase 🙂 I deal with such
info a lot. I was looking for this certain information for a very
lengthy time. Thanks and good luck.
What’s up, its nice piece of writing about media
print, we all be aware of media is a enormous source of facts.
Thanks for the good writeup. It if truth be told used to be a entertainment
account it. Look complicated to far added agreeable from you!
By the way, how could we keep up a correspondence?
I love your blog.. very nice colors & theme. Did
you create this website yourself or did you hire someone to do it for you?
Plz answer back as I’m looking to create my own blog and would
like to know where u got this from. thanks a lot
Thanks for sharing such a good thinking, paragraph is fastidious, thats
why i have read it completely
Hello! I could have sworn I’ve been to this website before but after reading through some
of the post I realized it’s new to me. Nonetheless, I’m definitely delighted I found
it and I’ll be bookmarking and checking back often!
Someone essentially help to make significantly articles I might state.
That is the very first time I frequented your website page
and up to now? I surprised with the analysis you made to make this
actual publish extraordinary. Fantastic job!
Quality content is the secret to interest the users
to pay a visit the website, that’s what this web site is providing.
Somebody essentially assist to make seriously articles
I’d state. This is the very first time I frequented your website page
and to this point? I surprised with the research you made to make this particular post amazing.
Great activity!
I will immediately seize your rss as I can not to find your e-mail subscription link or e-newsletter service.
Do you’ve any? Please let me know so that I may subscribe.
Thanks.
Hello, just wanted to mention, I enjoyed this post.
It was inspiring. Keep on posting!
It’s wonderful that you are getting thoughts from this piece of writing as well
as from our argument made at this time.
I every time emailed this webpage post page to all my associates, because if like to read it then my friends will too.
Hi there to all, how is everything, I think every one
is getting more from this web site, and your views
are nice for new users.
These are actually enormous ideas in regarding blogging.
You have touched some pleasant things here. Any
way keep up wrinting.
Hello there, I discovered your site by way of Google even as
searching for a similar matter, your website got here up, it seems great.
I have bookmarked it in my google bookmarks.
Hi there, simply turned into aware of your weblog through Google, and found
that it’s really informative. I’m going to be careful for brussels.
I’ll appreciate if you proceed this in future. A lot of people can be benefited out of your writing.
Cheers!
Hello, I log on to your new stuff daily. Your humoristic
style is awesome, keep doing what you’re doing!
Hi, this weekend is good in support of me, as this point in time i am reading this great educational post here at my house.
Hi! This is my first comment here so I just wanted to give a
quick shout out and tell you I really enjoy reading your blog posts.
Can you recommend any other blogs/websites/forums that go over
the same topics? Appreciate it!
Spot on with this write-up, I honestly believe that this amazing site needs
a lot more attention. I’ll probably be returning to
read more, thanks for the info!
Woah! I’m really loving the template/theme of this site.
It’s simple, yet effective. A lot of times it’s challenging
to get that “perfect balance” between usability and visual appearance.
I must say that you’ve done a excellent job with this. Additionally, the blog
loads very quick for me on Internet explorer. Superb Blog!
You’re so cool! I don’t think I have read through something like that before.
So nice to find somebody with unique thoughts on this issue.
Really.. many thanks for starting this up. This site is one thing that is needed on the web,
someone with some originality!
I’m not sure where you are getting your information, but great topic.
I needs to spend some time learning much more or understanding
more. Thanks for magnificent info I was looking for this info for my
mission.
Aw, this was a very nice post. Taking a few minutes and actual effort to create a top notch article…
but what can I say… I put things off a lot and never seem to get anything done.
We’re a group of volunteers and opening a brand
new scheme in our community. Your website provided
us with valuable information to work on. You
have performed an impressive process and our entire neighborhood can be thankful to
you.
Have you ever considered writing an ebook or guest authoring on other blogs?
I have a blog based upon on the same topics you discuss and would really like to have you share some stories/information. I know my visitors would
appreciate your work. If you are even remotely interested,
feel free to shoot me an e-mail.
It’s amazing to pay a quick visit this web page and reading the views of all colleagues concerning this piece of writing, while I am
also keen of getting know-how.
Hmm is anyone else having problems with the images on this
blog loading? I’m trying to find out if its a problem on my end or if it’s the blog.
Any suggestions would be greatly appreciated.
Everything is very open with a very clear clarification of the challenges.
It was truly informative. Your website is very useful.
Thanks for sharing!
It’s actually a nice and useful piece of information. I am happy
that you shared this useful info with us. Please stay us up to date like this.
Thank you for sharing.
Attractive part of content. I just stumbled upon your web site and in accession capital to assert that I get in fact loved account
your weblog posts. Any way I will be subscribing on your feeds or
even I fulfillment you get right of entry to persistently quickly.
Thanks , I have just been looking for information about this topic
for a while and yours is the greatest I’ve found out till now.
But, what in regards to the conclusion? Are you positive in regards to the source?
Thank you for the auspicious writeup. It actually was once a entertainment account it.
Glance advanced to far brought agreeable from you! However,
how can we keep up a correspondence?
I pay a visit each day some blogs and information sites to read
posts, but this web site gives quality based content.
These are actually impressive ideas in concerning blogging.
You have touched some pleasant things here. Any way
keep up wrinting.
Actually when someone doesn’t be aware of then its up to
other viewers that they will help, so here it happens.
Touche. Great arguments. Keep up the amazing spirit.
I am really impressed together with your writing abilities
and also with the format on your weblog. Is that
this a paid topic or did you customize it your self?
Anyway keep up the nice high quality writing, it is uncommon to see a nice blog like this one these days..
This text is worth everyone’s attention. When can I find out more?
Hi there, after reading this awesome article i am too happy to
share my knowledge here with colleagues.
Keep on working, great job!
Hi there to every , because I am genuinely keen of reading
this web site’s post to be updated daily. It carries good information.
This piece of writing is truly a pleasant one it helps new
the web viewers, who are wishing for blogging.
Great information. Lucky me I ran across your blog by accident (stumbleupon).
I have saved it for later!
I’ll immediately take hold of your rss as I can’t to find your e-mail subscription hyperlink or e-newsletter service.
Do you’ve any? Please let me realize so that I
may just subscribe. Thanks.
I am in fact thankful to the holder of this site who has shared this impressive piece of writing at here.
Fabulous, what a weblog it is! This webpage presents valuable facts to us, keep it up.
I have learn some just right stuff here. Certainly worth bookmarking for revisiting.
I wonder how much attempt you set to make this sort of wonderful informative web site.
This website certainly has all the information and facts I wanted concerning this subject and didn’t know who to ask.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your
point. You clearly know what youre talking about, why throw away your intelligence on just posting videos to your blog when you could be giving us something enlightening to read?
I do believe all the concepts you have offered to
your post. They’re really convincing and can certainly work.
Nonetheless, the posts are too short for beginners. May you
please lengthen them a bit from subsequent time?
Thank you for the post.
Howdy would you mind sharing which blog platform you’re using?
I’m planning to start my own blog in the near
future but I’m having a tough time selecting between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design and style seems
different then most blogs and I’m looking for something unique.
P.S Apologies for getting off-topic but I had to ask!
This blog was… how do you say it? Relevant!! Finally I have found something
that helped me. Many thanks!
I like the helpful information you provide in your articles.
I will bookmark your weblog and check again here regularly.
I am quite sure I’ll learn lots of new stuff right here!
Good luck for the next!
Hey there! I know this is kinda off topic but I was
wondering if you knew where I could locate a captcha plugin for my
comment form? I’m using the same blog platform
as yours and I’m having problems finding one? Thanks a lot!
Hey there! Do you know if they make any plugins to assist
with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good results.
If you know of any please share. Appreciate it!
Hi to every body, it’s my first pay a visit of this blog; this webpage contains remarkable and genuinely excellent data designed for readers.
This site was… how do I say it? Relevant!! Finally I have found something that helped
me. Cheers!
you’re in reality a excellent webmaster. The web site
loading velocity is amazing. It sort of feels that you’re doing any unique trick.
Moreover, The contents are masterpiece. you have performed a wonderful
process in this matter!
This paragraph is in fact a pleasant one it assists
new internet users, who are wishing in favor of blogging.
WOW just what I was looking for. Came here by searching for forum chat dewasa
It is perfect time to make a few plans for the long run and it
is time to be happy. I have read this put up and if I could I desire to suggest you few interesting things
or tips. Perhaps you can write subsequent articles relating to this article.
I wish to read more issues approximately it!
Keep this going please, great job!
I have read a few excellent stuff here. Certainly worth bookmarking for revisiting.
I surprise how so much effort you set to make any such excellent
informative site.
Hi, I do think this is an excellent site. I stumbledupon it 😉 I will revisit yet again since
I book marked it. Money and freedom is the greatest way to
change, may you be rich and continue to guide others.
This design is spectacular! You certainly
know how to keep a reader entertained. Between your wit and
your videos, I was almost moved to start my own blog (well, almost…HaHa!) Excellent
job. I really loved what you had to say, and more than that,
how you presented it. Too cool!
Pretty section of content. I just stumbled upon your site and in accession capital to assert that I get in fact enjoyed account your blog posts.
Anyway I’ll be subscribing to your augment and even I achievement you access consistently rapidly.
If you wish for to improve your familiarity simply keep visiting this web page
and be updated with the most recent news update posted here.
It’s not my first time to pay a visit this web page, i am visiting this web site dailly and obtain good data from here every day.
Ahaa, its pleasant dialogue regarding this post here at this weblog, I have read all that, so
now me also commenting at this place.
Its not my first time to pay a visit this web site, i am browsing this site dailly and take nice facts from here all
the time.
This information is priceless. When can I find out more?
My relatives every time say that I am killing my time
here at web, however I know I am getting familiarity every day by reading thes fastidious articles or reviews.
Heya i’m for the first time here. I came across this board and I find It
truly useful & it helped me out a lot. I hope to give something back and help others like
you aided me.
Heya i am for the first time here. I came across this board and
I find It truly useful & it helped me out much.
I hope to give something back and help others like you helped me.
Marvelous, what a weblog it is! This website
presents helpful data to us, keep it up.
Attractive section of content. I just stumbled upon your web site and in accession capital to assert that I get in fact enjoyed account your blog posts.
Anyway I’ll be subscribing to your feeds and even I achievement you access consistently rapidly.
It’s amazing to visit this web page and reading
the views of all colleagues about this paragraph, while I am also eager
of getting experience.
Hi this is somewhat of off topic but I was wondering if blogs use WYSIWYG editors or if you have to
manually code with HTML. I’m starting a blog soon but
have no coding knowledge so I wanted to get guidance from someone with experience.
Any help would be greatly appreciated!
I couldn’t refrain from commenting. Exceptionally well written!
I’m not sure exactly why but this site is loading incredibly slow for me.
Is anyone else having this issue or is it a issue on my end?
I’ll check back later on and see if the problem still exists.
This is a topic which is near to my heart… Best wishes!
Where are your contact details though?
I have read so many posts on the topic of the blogger lovers except this article is really a pleasant post, keep it up.
Everything is very open with a very clear description of
the challenges. It was definitely informative.
Your site is useful. Thank you for sharing!
Just want to say your article is as surprising. The clearness in your post is simply spectacular and i could assume you’re an expert on this
subject. Fine with your permission let me to grab your feed to keep up to date with forthcoming post.
Thanks a million and please carry on the enjoyable work.
This page definitely has all of the information and facts I wanted concerning
this subject and didn’t know who to ask.
Hey there, You’ve done a fantastic job. I’ll certainly digg
it and personally suggest to my friends. I am confident they will be benefited from this site.
You have made some decent points there. I checked on the web to find out
more about the issue and found most people will go
along with your views on this web site.
There’s certainly a lot to find out about this topic.
I like all of the points you have made.
My relatives every time say that I am wasting my time here at web, but I know I am getting know-how everyday
by reading such fastidious content.
I know this if off topic but I’m looking into starting my own blog and was wondering
what all is required to get setup? I’m assuming having a blog like yours would cost a pretty
penny? I’m not very web savvy so I’m not 100% certain. Any recommendations or advice
would be greatly appreciated. Cheers
It’s very trouble-free to find out any matter on net as
compared to textbooks, as I found this piece of writing at this website.
It’s impressive that you are getting ideas from this piece of writing as well as from our argument made at this place.
Greetings! This is my first comment here so I just wanted to give a quick shout out and say I genuinely enjoy reading your posts.
Can you recommend any other blogs/websites/forums that go
over the same topics? Thank you so much!
Thank you for the auspicious writeup. It in fact was a amusement account it.
Look advanced to more added agreeable from you! By the
way, how can we communicate?
First of all I would like to say excellent blog! I had a quick question in which I’d like to ask if you do not mind.
I was curious to know how you center yourself and
clear your mind prior to writing. I’ve had a hard time clearing my thoughts in getting my thoughts out there.
I truly do take pleasure in writing but it just seems like the first 10 to 15 minutes
tend to be wasted simply just trying to figure out how to begin. Any recommendations or tips?
Many thanks!
Hello There. I discovered your blog the usage of msn. This is a very
well written article. I will make sure to bookmark
it and return to read extra of your helpful information. Thank you for the
post. I’ll definitely comeback.
Hi there, just became alert to your blog through Google,
and found that it’s truly informative. I’m gonna watch out for brussels.
I’ll be grateful if you continue this in future.
A lot of people will be benefited from your writing.
Cheers!
Hi there just wanted to give you a quick heads up.
The words in your article seem to be running off the screen in Ie.
I’m not sure if this is a format issue or something to do with browser compatibility but I
figured I’d post to let you know. The layout look great though!
Hope you get the problem solved soon. Cheers
Pretty! This was a really wonderful post.
Thank you for providing this information.
naturally like your website however you need to take a look at the
spelling on several of your posts. Many of them are rife with spelling issues and
I in finding it very troublesome to tell the truth nevertheless I’ll surely come again again.
I just could not leave your site prior to suggesting that I really enjoyed the usual information a person supply
for your visitors? Is going to be again incessantly to check
out new posts
I am not sure where you’re getting your info, however good
topic. I must spend a while studying more or figuring out more.
Thank you for magnificent info I was looking for this info for my mission.
Just wish to say your article is as astonishing. The clarity in your
post is just cool and i could assume you’re an expert on this
subject. Well with your permission let me to grab your feed to keep up to date with forthcoming post.
Thanks a million and please carry on the
enjoyable work.
Wow, this paragraph is good, my younger
sister is analyzing these things, so I am going to tell her.
Superb blog! Do you have any recommendations
for aspiring writers? I’m hoping to start my own blog soon but I’m
a little lost on everything. Would you suggest starting with
a free platform like WordPress or go for a paid option? There are so many options out there
that I’m totally confused .. Any recommendations? Kudos!
Hello there! Do you use Twitter? I’d like to follow you if that would
be ok. I’m absolutely enjoying your blog and look forward to new posts.
I’ve been exploring for a little for any high quality articles or
blog posts on this kind of area . Exploring in Yahoo I ultimately stumbled upon this
website. Studying this info So i’m satisfied to express that I have
an incredibly just right uncanny feeling I discovered just what I needed.
I most definitely will make sure to do not forget this web site and
give it a look regularly.
Superb blog! Do you have any recommendations for aspiring writers?
I’m planning to start my own site soon but I’m a little lost on everything.
Would you advise starting with a free platform like WordPress or
go for a paid option? There are so many choices out there that I’m
totally overwhelmed .. Any suggestions? Bless you!
Do you have a spam issue on this site; I also am a blogger, and I was curious about your situation; many of us have developed some nice methods and we are looking
to exchange solutions with others, please shoot me an email if interested.
If some one wishes expert view regarding blogging and site-building afterward
i recommend him/her to visit this webpage, Keep up the good job.
I’m not sure where you’re getting your information,
but great topic. I needs to spend some time learning much more or understanding more.
Thanks for magnificent info I was looking for this info
for my mission.
It’s great that you are getting thoughts from this piece of writing as
well as from our discussion made at this time.
Good respond in return of this query with genuine arguments and
explaining all on the topic of that.
I’ve been browsing online more than three hours these days, but I by no means
discovered any attention-grabbing article like yours.
It’s lovely value sufficient for me. Personally, if all website owners and
bloggers made excellent content as you probably did, the web
will probably be a lot more useful than ever before.
I really like what you guys are up too. This sort of clever work and exposure!
Keep up the awesome works guys I’ve you guys to blogroll.
Hello, i think that i saw you visited my site so i came to “return the favor”.I’m attempting to find things to improve my web site!I suppose its ok to use some of your ideas!!
Quality content is the main to interest the visitors to pay a quick visit the web page, that’s what this
web site is providing.
Hello all, here every person is sharing such experience, thus it’s fastidious to read this blog, and I used to pay a visit this website all the time.
Hi there! I could have sworn I’ve been to this site before but after
browsing through some of the posts I realized it’s new to
me. Regardless, I’m certainly happy I stumbled upon it and I’ll be
book-marking it and checking back often!
There’s certainly a lot to find out about this topic.
I like all of the points you’ve made.
I am curious to find out what blog platform you’re utilizing?
I’m having some small security problems with my latest blog and I would like to find something more safeguarded.
Do you have any suggestions?
Hello, I enjoy reading through your article. I wanted to write
a little comment to support you.
I was excited to uncover this web site. I need to to thank
you for ones time just for this fantastic read!! I definitely appreciated every part of it and i also have you bookmarked to check out new stuff
in your website.
Good day! This is my first visit to your blog! We are a collection of volunteers and starting a new project in a community in the same niche.
Your blog provided us useful information to work on. You have
done a outstanding job!
I’m not sure why but this web site is loading extremely slow for me.
Is anyone else having this issue or is it a issue on my end?
I’ll check back later on and see if the problem still exists.
You should take part in a contest for one of the greatest websites on the net.
I most certainly will recommend this web site!
Hi to every body, it’s my first pay a quick visit of this
blog; this web site consists of awesome and genuinely good material in favor of visitors.
That is a very good tip especially to those fresh to the blogosphere.
Short but very accurate info… Many thanks for sharing
this one. A must read article!
magnificent issues altogether, you simply received a brand new reader.
What would you suggest in regards to your post that you made some days ago?
Any certain?
I savour, lead to I found just what I used to be having a look for.
You have ended my four day lengthy hunt! God Bless you man. Have a nice day.
Bye
Can I simply just say what a relief to uncover
a person that really understands what they’re discussing over the internet.
You certainly realize how to bring an issue to light and make it important.
More people must read this and understand this side of
your story. I was surprised that you are not more popular
given that you definitely possess the gift.
I am really enjoying the theme/design of your web site.
Do you ever run into any web browser compatibility issues?
A handful of my blog readers have complained about my
website not operating correctly in Explorer but looks great in Chrome.
Do you have any advice to help fix this problem?
I’m pretty pleased to uncover this site. I need to to thank
you for ones time for this wonderful read!! I definitely appreciated every part of it and i also have
you bookmarked to check out new things in your website.
I have to thank you for the efforts you have put
in writing this site. I am hoping to check out the same high-grade blog posts
by you in the future as well. In truth, your creative writing abilities
has encouraged me to get my very own site now 😉
My spouse and I stumbled over here coming from a different website and thought I should check
things out. I like what I see so now i am following you.
Look forward to exploring your web page repeatedly.
Paragraph writing is also a fun, if you know after that you can write if not
it is difficult to write.
This blog was… how do I say it? Relevant!!
Finally I’ve found something that helped me. Thanks a lot!
Incredible points. Sound arguments. Keep up
the amazing spirit.
This post presents clear idea in support of the new
visitors of blogging, that really how to do running a blog.
I don’t even know how I ended up here, but I thought this
post was good. I don’t know who you are but definitely you are going to a famous blogger if you aren’t already 😉
Cheers!
Everything is very open with a very clear clarification of the challenges.
It was definitely informative. Your website is
very helpful. Thanks for sharing!
You could certainly see your expertise in the work you write.
The sector hopes for even more passionate writers like you
who are not afraid to mention how they believe. All the time go after
your heart.
hey there and thank you for your info – I’ve definitely picked up anything new from right here.
I did however expertise several technical issues using this site, since I experienced to reload
the web site lots of times previous to I could get
it to load correctly. I had been wondering if your web host is
OK? Not that I’m complaining, but slow loading instances times will often affect your placement in google and can damage your high-quality score if advertising and marketing with Adwords.
Anyway I am adding this RSS to my e-mail and could look out for a
lot more of your respective exciting content. Ensure that you update this again very soon.
Hi, this weekend is fastidious designed for me, because this point in time i am
reading this wonderful educational piece of writing here at my house.
What a information of un-ambiguity and preserveness of valuable familiarity regarding unpredicted
emotions.
Everything is very open with a really clear clarification of the issues.
It was truly informative. Your site is useful. Thank you for sharing!
I’m extremely inspired along with your writing abilities and also with the layout in your blog.
Is this a paid theme or did you customize it your self?
Anyway stay up the excellent high quality writing,
it’s uncommon to look a nice weblog like this one today..
You ought to take part in a contest for one of the best blogs online.
I’m going to recommend this website!
You made some really good points there. I looked on the web for additional information about the issue and found most
people will go along with your views on this site.
fantastic put up, very informative. I wonder why the opposite experts
of this sector don’t realize this. You should continue your writing.
I’m sure, you’ve a huge readers’ base already!
Hello! I could have sworn I’ve been to this website before but after browsing through a few of the articles I realized it’s
new to me. Anyhow, I’m certainly happy I came across it and I’ll
be book-marking it and checking back frequently!
Thanks for ones marvelous posting! I certainly enjoyed reading it, you happen to be a great author.I will
be sure to bookmark your blog and will often come
back from now on. I want to encourage you to continue your great job, have a
nice afternoon!
Excellent blog here! Also your website loads up very fast!
What host are you using? Can I get your affiliate link
to your host? I wish my site loaded up as fast as yours lol
These are genuinely wonderful ideas in about blogging.
You have touched some fastidious things here.
Any way keep up wrinting.
I know this if off topic but I’m looking into starting my own blog
and was wondering what all is required to get set up?
I’m assuming having a blog like yours would cost a pretty
penny? I’m not very internet smart so I’m not 100% certain. Any tips or
advice would be greatly appreciated. Kudos
Wonderful work! This is the type of information that should
be shared across the web. Shame on Google for now not positioning this
post higher! Come on over and seek advice from my web site .
Thanks =)
This post is truly a nice one it assists
new net visitors, who are wishing for blogging.
Greate post. Keep writing such kind of information on your blog.
Im really impressed by it.
Hello there, You have done a great job. I’ll certainly digg it and for my part
recommend to my friends. I am sure they will be benefited from
this website.
What i don’t realize is actually how you are no longer really a lot more neatly-favored than you might be now.
You are very intelligent. You know thus considerably in terms of this subject, made me personally believe
it from so many varied angles. Its like men and women don’t seem to
be involved until it is something to accomplish with
Woman gaga! Your personal stuffs nice. At all times deal with
it up!
constantly i used to read smaller content that also clear their motive,
and that is also happening with this piece of
writing which I am reading at this place.
Hi there, There’s no doubt that your site may be having browser compatibility problems.
When I look at your web site in Safari, it looks fine but when opening in IE,
it’s got some overlapping issues. I merely wanted to provide
you with a quick heads up! Apart from that, great website!
My brother recommended I would possibly like this blog.
He was once entirely right. This publish truly made my day.
You cann’t consider just how much time I had spent for this
info! Thank you!
Wow! This blog looks exactly like my old one! It’s on a entirely different topic but it has pretty much the same page layout and design. Outstanding
choice of colors!
Great web site you have here.. It’s hard to find excellent writing like yours these days.
I really appreciate individuals like you! Take care!!
I’m not that much of a internet reader to be honest but your blogs really nice, keep it up!
I’ll go ahead and bookmark your site to come back later on. All
the best
I must thank you for the efforts you’ve put in writing this site.
I really hope to check out the same high-grade content by you
in the future as well. In fact, your creative writing abilities has motivated me to get my
very own blog now 😉
Attractive section of content. I just stumbled upon your weblog and in accession capital to assert that I get actually enjoyed account your blog posts.
Anyway I’ll be subscribing to your feeds and even I achievement you access consistently fast.
I was recommended this web site by my cousin. I am not sure whether this post
is written by him as nobody else know such detailed about my
trouble. You’re wonderful! Thanks!
It’s fantastic that you are getting thoughts from this piece of writing as well as from our dialogue made at this place.
I do not even know how I ended up here, but I thought this post was good.
I don’t know who you are but definitely you are going to a famous blogger if you are not already
😉 Cheers!
If some one wants to be updated with latest technologies after that he must be
pay a visit this site and be up to date all the time.
Sweet blog! I found it while surfing around on Yahoo
News. Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Appreciate it
you are in reality a just right webmaster. The web site loading velocity is amazing.
It sort of feels that you are doing any distinctive trick.
In addition, The contents are masterpiece.
you have performed a wonderful process on this matter!
Thanks for your personal marvelous posting! I seriously
enjoyed reading it, you happen to be a great author.
I will remember to bookmark your blog and will often come
back in the foreseeable future. I want to encourage
you continue your great job, have a nice evening!
After looking into a number of the articles on your web site, I truly like your technique
of blogging. I book-marked it to my bookmark website
list and will be checking back in the near future.
Please visit my web site as well and let me know
how you feel.
I have to thank you for the efforts you’ve put in writing this site.
I’m hoping to check out the same high-grade content by you later on as well.
In truth, your creative writing abilities has inspired
me to get my very own website now 😉
I’m not sure exactly why but this web site is
loading extremely slow for me. Is anyone else having this problem or is it a issue on my end?
I’ll check back later on and see if the problem still exists.
Thanks for sharing your thoughts about 4play to.
Regards
It’s actually very difficult in this full of activity life to listen news on Television,
thus I only use world wide web for that reason, and get the most
recent information.
Hey there! This post could not be written any better! Reading this post reminds me of my old room mate!
He always kept chatting about this. I will forward this article to him.
Pretty sure he will have a good read. Thank you for sharing!
I think this is one of the most significant information for
me. And i’m glad reading your article. But wanna remark on few general things,
The website style is wonderful, the articles is really great :
D. Good job, cheers
I do not even know how I ended up here, but I thought this post was great.
I do not know who you are but definitely you’re going to a famous blogger
if you aren’t already 😉 Cheers!
I really like your blog.. very nice colors
& theme. Did you make this website yourself or did you hire someone to do it
for you? Plz reply as I’m looking to construct my
own blog and would like to find out where u got this from.
thanks
Nice post. I was checking constantly this weblog and I
am impressed! Extremely useful info specially the remaining phase 🙂 I
take care of such info a lot. I used to be looking for this certain information for a long time.
Thanks and best of luck.
It’s perfect time to make some plans for the future and it’s time to be happy.
I have read this post and if I may I desire to counsel you some fascinating things or suggestions.
Perhaps you can write next articles referring
to this article. I want to learn more issues approximately it!
Thank you for sharing your info. I truly appreciate your efforts and I
will be waiting for your next write ups thanks once again.
Have you ever thought about creating an ebook or guest authoring
on other blogs? I have a blog centered on the same information you discuss and would really like
to have you share some stories/information. I know my readers would enjoy your work.
If you’re even remotely interested, feel free to shoot me an email.
Pretty nice post. I simply stumbled upon your blog and wished to say that I’ve truly loved browsing your weblog posts.
In any case I’ll be subscribing in your rss feed and I am
hoping you write once more very soon!
I was wondering if you ever considered changing the page layout of your site?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having one or 2 images.
Maybe you could space it out better?
It is appropriate time to make some plans for the future and it’s time to be happy.
I have read this post and if I could I desire to suggest you some
interesting things or suggestions. Perhaps you can write next
articles referring to this article. I wish to read more things about it!
We stumbled over here different web page and thought I may
as well check things out. I like what I see so now i’m
following you. Look forward to going over your web page again.
Asking questions are genuinely fastidious thing if you are not understanding something
fully, however this piece of writing offers good understanding yet.
What’s up mates, nice piece of writing and fastidious urging commented here, I am actually enjoying by
these.
It’s remarkable designed for me to have a website, which is valuable in favor of my experience.
thanks admin
Please let me know if you’re looking for a article author for your weblog.
You have some really good posts and I feel I would be a good asset.
If you ever want to take some of the load off, I’d love to write some material for your blog in exchange for a link back to mine.
Please blast me an e-mail if interested. Many thanks!
I enjoy, lead to I discovered exactly what I was looking for.
You’ve ended my 4 day lengthy hunt! God Bless you man. Have a great day.
Bye
You actually make it seem so easy with your presentation but I find this topic to be actually something which I think I
would never understand. It seems too complicated and very broad for me.
I am looking forward for your next post, I will try
to get the hang of it!
Hello mates, how is the whole thing, and what you want to say on the topic of this paragraph, in my
view its truly awesome designed for me.
Spot on with this write-up, I seriously think this site needs a great deal more attention. I’ll probably be back again to read
through more, thanks for the advice!
Do you mind if I quote a few of your articles as long as I provide credit and sources
back to your weblog? My blog is in the exact same niche as yours and my users would really benefit from some of
the information you provide here. Please let me know if
this ok with you. Thanks a lot!
This piece of writing is really a good one
it assists new the web viewers, who are wishing in favor of
blogging.
I do believe all the ideas you have presented to your post.
They are really convincing and can definitely work.
Nonetheless, the posts are too brief for beginners.
May just you please lengthen them a bit from next time?
Thanks for the post.
Do you have a spam problem on this website; I also am a blogger, and I was wondering your situation; many of us have created some nice practices and we
are looking to exchange techniques with other folks, why not
shoot me an email if interested.
This is a topic that’s close to my heart… Thank you!
Exactly where are your contact details though?
You made some good points there. I checked on the web for more information about the issue and found most
individuals will go along with your views on this site.
Valuable information. Lucky me I found your website accidentally, and I’m stunned
why this accident did not came about in advance! I bookmarked it.
Hello! I’m at work surfing around your blog from my new iphone
4! Just wanted to say I love reading your blog and look forward to all your
posts! Carry on the excellent work!
I’ve read a few just right stuff here. Certainly value bookmarking for revisiting.
I surprise how a lot attempt you place to create any such excellent informative site.
If you wish for to increase your experience only keep visiting this web
page and be updated with the most recent information posted here.
Great post. I used to be checking continuously this blog
and I’m inspired! Very useful info specifically the closing phase 🙂 I maintain such info much.
I was seeking this particular info for a very long time. Thank
you and best of luck.
What’s up i am kavin, its my first occasion to commenting anyplace, when i read this piece of
writing i thought i could also make comment due to this good article.
Greate article. Keep posting such kind of info on your page.
Im really impressed by it.
Hi there, You’ve performed a fantastic job. I’ll certainly digg it and in my view suggest to my friends.
I am sure they will be benefited from this website.
Incredible points. Outstanding arguments. Keep up
the good effort.
Really when someone doesn’t know afterward its up to other visitors that they will assist,
so here it occurs.
If some one needs expert view about blogging and site-building after that i
recommend him/her to pay a visit this blog, Keep up the pleasant work.
fantastic points altogether, you just received a brand new reader.
What might you recommend about your submit that you made a few days in the past?
Any positive?
It’s a shame you don’t have a donate button! I’d certainly donate to this outstanding blog!
I suppose for now i’ll settle for bookmarking and adding
your RSS feed to my Google account. I look forward to brand
new updates and will share this website with my
Facebook group. Talk soon!
Do you mind if I quote a couple of your articles as long as I provide credit and sources back to your blog?
My blog site is in the exact same area of interest as yours and
my visitors would really benefit from some of the information you
provide here. Please let me know if this okay with you. Many thanks!
You have made some decent points there. I checked on the web to learn more about the issue and found most individuals will go along with your views on this site.
Hello, after reading this amazing post i am also happy to share my familiarity here with colleagues.
If some one wishes expert view regarding blogging then i propose him/her to visit this webpage, Keep up
the good work.
Hi, i think that i saw you visited my website so i came to “return the favor”.I’m attempting to find things to improve my
web site!I suppose its ok to use some of your ideas!!
I used to be able to find good info from your articles.
Thank you, I’ve recently been looking for information approximately this topic
for ages and yours is the best I’ve came upon so far.
But, what about the conclusion? Are you certain concerning the source?
I don’t even know how I ended up here, but I thought
this post was good. I do not know who you
are but definitely you’re going to a famous blogger if you are not
already 😉 Cheers!
I feel this is one of the so much important info for me.
And i’m satisfied studying your article. However should statement
on some general things, The web site taste is perfect, the articles is really nice : D.
Just right activity, cheers
Have you ever considered publishing an ebook or guest authoring on other blogs?
I have a blog based on the same information you discuss and would really like
to have you share some stories/information. I know my visitors would enjoy your work.
If you’re even remotely interested, feel free to shoot me an e-mail.
I’m not sure why but this blog is loading very slow
for me. Is anyone else having this issue or is it a problem
on my end? I’ll check back later on and see if the problem still exists.
Simply wish to say your article is as amazing. The clarity in your post is simply great and i could assume you’re an expert on this subject.
Fine with your permission let me to grab your
RSS feed to keep up to date with forthcoming post. Thanks a million and please keep up the gratifying work.
An interesting discussion is worth comment. I think that you should
publish more on this subject, it might not be a taboo matter but generally people don’t speak about these
subjects. To the next! Kind regards!!
Hiya! I know this is kinda off topic nevertheless I’d figured
I’d ask. Would you be interested in trading links
or maybe guest authoring a blog article or vice-versa?
My site addresses a lot of the same topics as yours and I feel we could greatly benefit from each other.
If you’re interested feel free to shoot me an email.
I look forward to hearing from you! Terrific blog by the way!
Thank you for the good writeup. It in truth used to be a leisure account it.
Look complex to far brought agreeable from you! By the way, how can we keep up a correspondence?
Oh my goodness! Incredible article dude! Thank you, However I am experiencing issues with your RSS.
I don’t know why I can’t subscribe to it. Is there anyone else having similar
RSS issues? Anyone who knows the answer can you kindly respond?
Thanx!!
You should take part in a contest for one of the highest quality sites online.
I am going to recommend this site!
Heya! I understand this is kind of off-topic however I had to ask.
Does managing a well-established website like yours require a lot of work?
I am brand new to running a blog but I do write in my diary everyday.
I’d like to start a blog so I can easily share
my personal experience and feelings online. Please let me know if you have any suggestions or tips for brand new aspiring
blog owners. Thankyou!
Yes! Finally someone writes about situs bokep.
I have been browsing online more than 2 hours today,
yet I never found any interesting article like yours.
It is pretty worth enough for me. In my opinion, if all website owners and
bloggers made good content as you did, the web will be much more
useful than ever before.
Howdy are using WordPress for your blog platform?
I’m new to the blog world but I’m trying to get
started and create my own. Do you need any coding knowledge to make your
own blog? Any help would be greatly appreciated!
Normally I don’t learn article on blogs, but I wish to say that this write-up very pressured me to check out and do so!
Your writing taste has been amazed me. Thank you, very
great article.
Undeniably believe that that you stated. Your favorite reason seemed to be at the internet the easiest
thing to consider of. I say to you, I definitely get irked whilst
folks consider concerns that they just do not know about.
You managed to hit the nail upon the top and defined out the whole thing with no need side-effects
, other people could take a signal. Will likely be back to get
more. Thanks
I was extremely pleased to uncover this web site. I wanted to thank you for
ones time for this particularly wonderful read!!
I definitely really liked every part of it and i also have you bookmarked
to check out new information on your blog.
I just like the helpful information you supply on your articles.
I will bookmark your blog and take a look at once more right here
regularly. I am reasonably sure I will learn many new stuff
right here! Good luck for the next!
For latest news you have to pay a visit world-wide-web and on the web
I found this web page as a best web page for newest updates.
I read this piece of writing fully on the topic of the difference of most up-to-date and earlier technologies,
it’s awesome article.
Hello there! This post couldn’t be written any better! Reading
this post reminds me of my good old room mate!
He always kept talking about this. I will forward this page to him.
Fairly certain he will have a good read. Thank you for sharing!
It’s the best time to make a few plans for the future and it’s
time to be happy. I have learn this put up and if I may I desire
to suggest you some interesting things or tips. Maybe you could write next articles regarding this article.
I want to read more issues about it!
Very good blog post. I absolutely appreciate this
website. Thanks!
Wonderful article! We are linking to this great article on our site.
Keep up the great writing.
I enjoy what you guys are usually up too. This type of clever work and exposure!
Keep up the amazing works guys I’ve you guys to my blogroll.
It’s perfect time to make a few plans for the long run and it is time to be happy.
I’ve learn this post and if I may just I desire to counsel
you few interesting things or tips. Perhaps you can write next articles
relating to this article. I want to read more issues approximately it!
Hey there! I know this is kinda off topic nevertheless I’d figured I’d ask.
Would you be interested in trading links or maybe guest authoring a blog post or vice-versa?
My blog addresses a lot of the same subjects as yours
and I believe we could greatly benefit from each other.
If you might be interested feel free to shoot me an email.
I look forward to hearing from you! Awesome blog by the way!
Hi would you mind stating which blog platform you’re working with?
I’m planning to start my own blog in the near future but I’m having a difficult time choosing between BlogEngine/Wordpress/B2evolution and
Drupal. The reason I ask is because your design and style seems different then most blogs
and I’m looking for something unique.
P.S Sorry for getting off-topic but I had to ask!
Hi there to every body, it’s my first pay a quick visit
of this weblog; this weblog includes amazing and actually good stuff for visitors.
Spot on with this write-up, I seriously believe this amazing site needs a great deal more attention.
I’ll probably be returning to read more, thanks for the info!
I was wondering if you ever thought of changing the structure of your site?
Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people
could connect with it better. Youve got an awful lot of text for only having one or 2 images.
Maybe you could space it out better?
Normally I do not learn post on blogs, but I would like to say that this write-up very compelled me to take a
look at and do so! Your writing style has been amazed me.
Thanks, very great post.
I got this web site from my buddy who told me regarding this web page and at the
moment this time I am visiting this site and reading very informative articles at this
time.
Definitely believe that which you said. Your favorite reason seemed to be on the internet the simplest thing to be
aware of. I say to you, I definitely get annoyed while people
think about worries that they plainly do not know about.
You managed to hit the nail upon the top and defined out the whole thing without having side effect , people could
take a signal. Will likely be back to get more. Thanks
I like the valuable information you provide in your articles.
I will bookmark your weblog and check again here regularly.
I’m quite sure I will learn a lot of new stuff right here!
Good luck for the next!
I like the valuable information you provide in your articles.
I will bookmark your blog and check again here regularly.
I’m quite sure I’ll learn many new stuff right here!
Best of luck for the next!
Hi to all, the contents existing at this web site are really
awesome for people experience, well, keep up the nice work fellows.
You made some really good points there. I checked on the internet for additional information about
the issue and found most individuals will go along with your views on this web site.
Excellent post. I was checking continuously this blog and I am impressed!
Extremely helpful info specially the last part 🙂 I
care for such information a lot. I was seeking this
particular info for a long time. Thank you and good luck.
Excellent, what a web site it is! This web site gives useful data
to us, keep it up.
We are a group of volunteers and opening a brand new scheme in our
community. Your website provided us with useful
info to work on. You’ve performed an impressive activity and our entire group can be thankful to you.
Sweet blog! I found it while browsing on Yahoo News.
Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Cheers
Appreciate this post. Will try it out.
My brother suggested I might like this blog. He was totally right.
This post truly made my day. You cann’t imagine simply how
much time I had spent for this info! Thanks!
I know this site gives quality dependent articles or reviews
and extra information, is there any other website which provides such stuff in quality?
I have been exploring for a little for any high quality articles or weblog posts in this sort of house .
Exploring in Yahoo I finally stumbled upon this website.
Studying this info So i’m satisfied to convey that I’ve a very
good uncanny feeling I discovered exactly what I needed. I such a lot no doubt will make sure to do not put out of your mind this website and give it
a glance regularly.
Awesome! Its actually remarkable paragraph, I have got
much clear idea on the topic of from this article.
We are a group of volunteers and starting a new scheme in our community.
Your site offered us with valuable info to work on. You’ve done a formidable job and our whole community will be thankful to you.
Hello my friend! I wish to say that this post is amazing,
great written and include approximately all significant infos.
I’d like to peer more posts like this .
WOW just what I was searching for. Came here by searching for bokep abg
WOW just what I was searching for. Came here by searching for
forum lendir semarang
Unquestionably imagine that which you stated.
Your favourite reason seemed to be at the internet the easiest factor to be mindful of.
I say to you, I certainly get annoyed even as other folks think about concerns that they plainly don’t recognise about.
You controlled to hit the nail upon the top and also defined out the whole thing
with no need side effect , other people could take a signal.
Will probably be back to get more. Thanks
Hi there! Would you mind if I share your blog with my
twitter group? There’s a lot of folks that I
think would really enjoy your content. Please let me know.
Thank you
I every time spent my half an hour to read this
web site’s articles all the time along with a cup of
coffee.
I do believe all of the ideas you have introduced on your post.
They’re very convincing and will definitely work.
Nonetheless, the posts are too brief for beginners. May you please
extend them a little from subsequent time?
Thanks for the post.
Keep on writing, great job!
I’m curious to find out what blog system you happen to be utilizing?
I’m experiencing some minor security problems with my latest site and I’d like to
find something more secure. Do you have any solutions?
This design is incredible! You definitely know
how to keep a reader entertained. Between your wit and your
videos, I was almost moved to start my own blog (well, almost…HaHa!) Fantastic job.
I really loved what you had to say, and more than that, how you presented it.
Too cool!
Hi there to every one, it’s really a nice for
me to pay a visit this web site, it contains precious Information.
Wow, this paragraph is nice, my younger sister is analyzing these kinds of things, therefore I am going to inform her.
Fine way of describing, and fastidious article to take information about my presentation subject matter, which i am going to deliver in university.
Hello there, You’ve done an incredible job. I will definitely digg it and personally
suggest to my friends. I’m sure they will be benefited from this site.
It is in point of fact a nice and helpful piece of information. I am
happy that you just shared this helpful information with us.
Please stay us informed like this. Thank you for sharing.
Hmm is anyone else experiencing problems with the pictures on this blog loading?
I’m trying to figure out if its a problem on my end or if
it’s the blog. Any suggestions would be greatly
appreciated.
It’s genuinely very complex in this full of activity life to
listen news on Television, thus I simply use the web for that reason, and get the
most recent information.
It’s an remarkable post in support of all the online people;
they will obtain benefit from it I am sure.
Great blog here! Also your website loads up very fast! What
web host are you using? Can I get your affiliate link to your host?
I wish my site loaded up as quickly as yours lol
Heya i’m for the primary time here. I came across this board and I find It really helpful
& it helped me out a lot. I’m hoping to give one thing back and aid others such as you aided me.
If you desire to obtain much from this paragraph then you have
to apply these methods to your won blog.
I’m extremely impressed with your writing skills as well as with the layout
on your weblog. Is this a paid theme or did you modify it yourself?
Anyway keep up the nice quality writing, it’s rare to
see a great blog like this one these days.
I’m impressed, I have to admit. Rarely do I encounter a blog that’s both equally educative and entertaining, and
without a doubt, you have hit the nail on the head.
The problem is something that too few men and women are speaking intelligently
about. I am very happy I came across this during my search for something concerning this.
I pay a visit day-to-day a few websites and sites to read articles
or reviews, but this blog presents quality based writing.
I think that is among the so much significant
info for me. And i am satisfied studying your article.
However want to commentary on few common things, The web
site style is wonderful, the articles is really great : D.
Good process, cheers
Thanks for another magnificent post. Where else could anyone get that kind of information in such
a perfect way of writing? I’ve a presentation next week, and I am
on the search for such info.
Thank you for the auspicious writeup. It in fact was a
amusement account it. Look advanced to more added agreeable from you!
By the way, how could we communicate?
I like looking through a post that can make men and women think.
Also, thanks for allowing for me to comment!
Fine way of telling, and pleasant piece of writing to take facts
on the topic of my presentation focus, which i am going to deliver in school.
Wow that was odd. I just wrote an really long comment but after I
clicked submit my comment didn’t appear. Grrrr…
well I’m not writing all that over again. Regardless, just wanted to say fantastic blog!
I don’t even know how I ended up here, but
I thought this post was good. I don’t know who you
are but definitely you’re going to a famous blogger if you are
not already 😉 Cheers!
Great site you have here.. It’s hard to find excellent writing like
yours nowadays. I seriously appreciate individuals like you!
Take care!!
Howdy would you mind sharing which blog platform you’re using?
I’m looking to start my own blog in the near future but I’m having a hard time making a
decision between BlogEngine/Wordpress/B2evolution and
Drupal. The reason I ask is because your design seems
different then most blogs and I’m looking for something unique.
P.S My apologies for being off-topic but
I had to ask!
Your mode of telling the whole thing in this paragraph is actually nice, every
one be capable of simply know it, Thanks a lot.
– Я не получаю то, что хочу.
– Не хватает мотивации на регулярные занятия.
– Мои цели сбываются у других людей.
Почему так, проконсультируйся у опсуимолога!
Вбивай в поиск: “опсуимолог” и получи актуальные контакты.
Ты же знаешь кто такой опсуимолог?
Nice blog here! Also your site loads up fast! What host are you using?
Can I get your affiliate link to your host? I wish my website loaded up as fast as yours lol
I every time spent my half an hour to read this web
site’s posts everyday along with a cup of coffee.
If you want to improve your familiarity only keep visiting this web page and be
updated with the newest news posted here.
Can you tell us more about this? I’d love to find out some additional information.
Excellent weblog right here! Also your website rather a lot up fast!
What web host are you the use of? Can I get your affiliate hyperlink
in your host? I want my website loaded up as quickly as yours
lol
Can you tell us more about this? I’d like to find out more details.
Hey there, You’ve done an incredible job. I will certainly digg it and personally suggest to
my friends. I am confident they’ll be benefited from
this web site.
It’s actually a cool and useful piece of info. I’m happy that you simply shared this helpful information with us.
Please keep us up to date like this. Thanks for sharing.
This is a topic which is close to my heart… Take care!
Where are your contact details though?
My partner and I stumbled over here from a different website and thought I might as well check
things out. I like what I see so now i’m following you.
Look forward to finding out about your web page yet again.
Today, I went to the beach front with my kids. I found a sea shell
and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She
placed the shell to her ear and screamed. There was a hermit
crab inside and it pinched her ear. She never wants to go back!
LoL I know this is totally off topic but I had to tell someone!
Truly no matter if someone doesn’t be aware of afterward its up to other people
that they will help, so here it takes place.
A person essentially help to make seriously articles I would state.
This is the very first time I frequented your website page and so far?
I amazed with the analysis you made to create this actual submit amazing.
Great task!
Hi there to every body, it’s my first go to see of this weblog; this weblog includes awesome
and really fine information designed for readers.
Greetings from California! I’m bored at work so I decided to browse your
blog on my iphone during lunch break. I really like the information you present here and can’t wait to take a
look when I get home. I’m shocked at how
quick your blog loaded on my mobile .. I’m not even using WIFI, just
3G .. Anyhow, fantastic blog!
Your style is unique compared to other people I have read stuff from.
Thank you for posting when you have the opportunity,
Guess I’ll just bookmark this page.
Hi there! Someone in my Myspace group shared this site with us so I came to look it over.
I’m definitely loving the information. I’m book-marking and
will be tweeting this to my followers! Excellent blog and terrific
design and style.
Greetings! I’ve been reading your blog for a while now and finally got the bravery
to go ahead and give you a shout out from Atascocita Texas!
Just wanted to mention keep up the good job!
Thank you, I’ve just been searching for information about this topic for a while and yours is the greatest I
have found out till now. However, what in regards to the conclusion? Are you certain concerning the source?
I am sure this post has touched all the internet users,
its really really pleasant post on building up new
web site.
Hey there! This is my first visit to your blog! We are a
group of volunteers and starting a new initiative in a community
in the same niche. Your blog provided us beneficial information to work on. You have done a outstanding job!
I used to be able to find good info from your
blog posts.
Definitely believe that which you said. Your favorite justification seemed to
be on the internet the easiest thing to be aware
of. I say to you, I certainly get annoyed while people think about worries that they just do not know about.
You managed to hit the nail upon the top as well as defined out the whole thing without
having side effect , people can take a signal. Will likely be back to get more.
Thanks
I’ve been browsing online greater than three hours these
days, yet I by no means found any fascinating article like yours.
It is pretty worth enough for me. In my view, if all webmasters and bloggers made just right content as you did,
the web will likely be a lot more useful than ever before.
I was wondering if you ever considered changing the page layout of
your website? Its very well written; I love what youve got to say.
But maybe you could a little more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having 1 or two pictures.
Maybe you could space it out better?
Undeniably believe that which you stated. Your favorite justification seemed to be on the internet
the simplest thing to be aware of. I say to you, I definitely get annoyed while people think about worries
that they just do not know about. You managed to hit the nail upon the
top and defined out the whole thing without having side-effects ,
people could take a signal. Will probably be back to get more.
Thanks
Hi there, every time i used to check blog posts here early
in the break of day, since i love to find out more and
more.
Have you ever thought about including a little bit more than just
your articles? I mean, what you say is valuable and everything.
But just imagine if you added some great images or video clips to give your
posts more, “pop”! Your content is excellent but with pics and video clips, this site could definitely be one of the most beneficial in its field.
Very good blog!
Great work! This is the kind of info that are meant to be shared across the web.
Disgrace on the search engines for no longer positioning this post upper!
Come on over and seek advice from my website . Thanks =)
always i used to read smaller articles that also clear their motive, and that is also happening with this post which I am reading here.
you are in reality a just right webmaster.
The web site loading pace is amazing. It seems that you’re
doing any unique trick. In addition, The contents are masterwork.
you’ve done a excellent job on this matter!
Hi there, I found your web site via Google while searching for a related topic, your website came up, it seems great.
I have bookmarked it in my google bookmarks.
Hi there, simply changed into alert to your blog through Google, and
found that it is truly informative. I’m gonna be careful for brussels.
I’ll be grateful in case you proceed this in future. Many
people will probably be benefited from your writing.
Cheers!
Really when someone doesn’t be aware of then its up to other people that they will help, so
here it happens.
I believe that is one of the most significant info for me.
And i am satisfied reading your article. But wanna observation on few common issues, The website style is
perfect, the articles is actually great : D. Good task, cheers
Terrific article! This is the kind of information that are meant to be
shared around the internet. Shame on the search engines for not positioning this put up upper!
Come on over and visit my site . Thank you =)
I’ve been exploring for a little for any high
quality articles or weblog posts on this kind of area . Exploring
in Yahoo I finally stumbled upon this web site.
Studying this info So i am satisfied to express that I have a very excellent
uncanny feeling I found out exactly what I needed.
I such a lot definitely will make sure to do not omit this site and provides it a
look regularly.
I am not positive where you are getting your info, however great topic.
I must spend a while learning much more or working out more.
Thank you for great information I was searching for
this information for my mission.
I am sure this piece of writing has touched all the internet visitors, its really really good piece of writing on building up new
weblog.
I’m amazed, I must say. Seldom do I encounter
a blog that’s both educative and entertaining, and let
me tell you, you’ve hit the nail on the head. The issue is an issue that too few people are speaking intelligently about.
I am very happy that I came across this during my search for something regarding this.
Hey there! I know this is kinda off topic but I’d figured I’d ask.
Would you be interested in trading links or maybe guest writing a blog article or vice-versa?
My blog addresses a lot of the same topics as yours and I think we could greatly
benefit from each other. If you are interested feel free to
shoot me an e-mail. I look forward to hearing from you!
Fantastic blog by the way!
I blog frequently and I truly appreciate your
information. The article has really peaked my interest.
I will take a note of your website and keep checking for new details about once
per week. I subscribed to your Feed as well.
Pretty great post. I just stumbled upon your blog and wished to mention that I have really loved browsing your weblog posts.
In any case I will be subscribing on your feed and I hope you write once more very soon!
Hello! I know this is kind of off topic but I was wondering which blog platform are you using for this website?
I’m getting tired of WordPress because I’ve had problems with hackers and I’m
looking at alternatives for another platform. I would be awesome if you could point
me in the direction of a good platform.
Hello, all the time i used to check webpage posts here early in the morning, since i like to
gain knowledge of more and more.
Oh my goodness! Amazing article dude! Many thanks, However I am experiencing problems with your RSS.
I don’t know why I can’t subscribe to it. Is there anybody else having similar RSS problems?
Anyone that knows the solution can you kindly respond?
Thanx!!
I know this if off topic but I’m looking into
starting my own blog and was curious what all is required to get setup?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet smart so I’m not 100% certain. Any suggestions
or advice would be greatly appreciated. Kudos
Interesting blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple tweeks would really make my
blog stand out. Please let me know where you got your design. Thanks a lot
I all the time used to read paragraph in news papers but
now as I am a user of net therefore from now I am using net for articles or reviews, thanks to web.
Hey there! I’m at work browsing your blog from my new iphone!
Just wanted to say I love reading your blog and look forward
to all your posts! Carry on the fantastic work!
Hey there! Someone in my Myspace group shared this site with us so I came to give it a
look. I’m definitely enjoying the information. I’m bookmarking and will be tweeting this to my followers!
Exceptional blog and fantastic style and design.
Hello, i think that i saw you visited my web site so
i came to “return the favor”.I am attempting to find things to enhance my web site!I
suppose its ok to use a few of your ideas!!
Hello to all, how is the whole thing, I think every one is getting more from this web site,
and your views are nice designed for new viewers.
I am sure this piece of writing has touched all the internet users,
its really really good piece of writing on building up new
blog.
Howdy! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m
not seeing very good results. If you know of
any please share. Thanks!
Hi, I do believe this is a great blog. I stumbledupon it 😉 I will come back yet again since I
saved as a favorite it. Money and freedom is
the greatest way to change, may you be rich and
continue to help other people.
Hi Dear, are you actually visiting this site regularly, if so afterward
you will without doubt obtain pleasant knowledge.
Magnificent items from you, man. I’ve be aware your stuff previous to
and you’re just extremely magnificent. I really like
what you’ve received right here, really like what you are stating and the way
in which during which you say it. You make
it entertaining and you continue to care for to stay it smart.
I can’t wait to read much more from you. That is actually a great web site.
This is the right website for anybody who wishes to understand this topic.
You understand a whole lot its almost hard to argue with you
(not that I actually would want to…HaHa). You definitely put a fresh spin on a subject that’s been written about for decades.
Excellent stuff, just excellent!
What’s up, constantly i used to check blog posts here early in the daylight, since i
like to find out more and more.
Howdy! Do you use Twitter? I’d like to follow you if that would be ok.
I’m definitely enjoying your blog and look forward to new updates.
I don’t even understand how I stopped up right here,
however I believed this submit used to be good. I don’t recognize who you might be however certainly you are
going to a famous blogger should you aren’t already. Cheers!
Vladimir Putin Putin Carlson Interview.
Vladimir Putin.
This info is priceless. When can I find out more?
Hey! I realize this is somewhat off-topic but I had to ask.
Does building a well-established blog such as yours require a
lot of work? I am completely new to operating a blog but I do write in my journal every day.
I’d like to start a blog so I can share my experience and views online.
Please let me know if you have any kind of ideas or tips
for new aspiring blog owners. Appreciate it!
Greetings! Very useful advice within this post! It’s the little changes that will make the biggest changes.
Many thanks for sharing!
Skillful leaders know how to balance working on relationships and
strengthening formal status and authority. Both components need to be developed.
The best site about relationship
Ad usum populi — Для народного употребления.
Causa finita est — Дело кончено, вопрос решён.
Hey there! Someone in my Myspace group shared this site with us so I came to give it
a look. I’m definitely enjoying the information. I’m bookmarking and will be
tweeting this to my followers! Superb blog and terrific design.
First of all I want to say excellent blog! I had a quick question in which I’d like to
ask if you do not mind. I was curious to know how you center yourself
and clear your head before writing. I have had a difficult time clearing my mind in getting my ideas out.
I do take pleasure in writing however it just seems like the first 10 to 15 minutes are wasted simply just trying to
figure out how to begin. Any recommendations or hints?
Many thanks!
Я хотел бы подчеркнуть четкость и последовательность изложения в этой статье. Автор сумел объединить информацию в понятный и логичный рассказ, что помогло мне лучше усвоить материал. Очень ценная статья!
For latest information you have to visit world-wide-web and
on web I found this site as a best web page for most recent updates.
Pretty! This was a really wonderful post. Thank you for supplying these details.
It’s very interesting! If you need help, look here: ARA Agency
Я очень доволен, что прочитал эту статью. Она оказалась настоящим открытием для меня. Информация была представлена в увлекательной и понятной форме, и я получил много новых знаний. Спасибо автору за такое удивительное чтение!
Полезно, что автор предоставил разные точки зрения на обсуждаемую тему.
Читателям предоставляется возможность ознакомиться с различными аспектами темы и сделать собственные выводы.
Я оцениваю точность и достоверность фактов, представленных в статье.
Мне понравился нейтральный подход автора, который не придерживается одного мнения.
Marvelous, what a weblog it is! This weblog gives useful information to us, keep it up.
I think this is one of the most important information for me. And i am glad reading your article. But should remark on some general things, The website style is wonderful, the articles is really nice : D. Good job, cheers
Мне понравился нейтральный тон статьи, который позволяет читателю самостоятельно сформировать мнение.
Хорошая статья, которая основана на фактах и не сторонится от нейтральности.
Приятно видеть объективный подход и анализ проблемы без сильного влияния субъективных факторов.
Great blog here! Also your web site loads up
fast! What host are you using? Can I get your
affiliate link to your host? I wish my web
site loaded up as quickly as yours lol
g-u.su
Hi there to all, for the reason that I am truly keen of reading
this website’s post to be updated regularly. It includes pleasant data.
Good day! Do you use Twitter? I’d like to follow you if that would
be ok. I’m undoubtedly enjoying your blog and look forward to new posts.
Hi there, after reading this awesome piece of writing i am
as well happy to share my know-how here with friends.
Following point we will certainly do is create a comprehensive write-up, spin it, and add it into GSA SER.
Also visit my homepage … https://www.facebook.com/serverifiedlists/
You generally obtain a DEMONSTRATION VERSION when you initially examine GSA SEO Indexer.
Here is my web page – https://medium.com/@traveltoday0082/unlocking-the-full-potential-of-gsa-search-engine-ranker-for-seo-mastery-69fb8e100768
Wow, awesome blog structure! How lengthy have you
ever been running a blog for? you make running a blog glance easy.
The whole look of your website is excellent, as neatly as the content material!
It includes it such as this at the bottom this sentence here, it resembles an arbitrary sentence that it includes.
Here is my site: https://www.reddit.com/r/SEOStrategiesHub/comments/1bunt6n/mastering_gsa_ser_a_guide_to_best_practices_for/
This software application can run endlessly and develop backlinks for you 7 days a week.
Also visit my webpage – https://www.peilex.com/2014/02/13/osservatorio-infrastrutture/
There are all sorts of bets you can spot at American Roulette, such as split bets, street bets, corner bets, and column bets.
Visit my webpage … https://kobet.co.kr/%EC%83%88%EB%A1%9C%EC%9A%B4-%EC%84%B8%EA%B3%84%EB%A1%9C%EC%9D%98-%EC%B4%88%EB%8C%80-%EC%B9%B4%EC%A7%80%EB%85%B8-%EA%B0%80%EC%9E%85-%EB%B0%A9%EB%B2%95/
If you desire to improve your knowledge only keep visiting
this site and be updated with the latest news posted here.
This is my first time pay a quick visit at here and i am in fact happy to read everthing at alone
place.
I’m gone to tell my little brother, that he should also pay a visit this blog on regular basis to get updated
from latest news update.
Fascinating blog! Is your theme custom made or did you download it from somewhere?
A theme like yours with a few simple adjustements would really make my
blog jump out. Please let me know where you got your design. With thanks
Terrific write ups. Cheers!
Feel free to surf to my web site – https://godayjob.com/2024/04/06/welcome-to-the-top-online-casinos-in-korea/
Line up the wager you are prepared to stake and confirm the transaction.
Here is my blog – https://Godayjob.com/2024/04/13/unlock-exciting-korean-betting-site-bonuses-today/
Remarkable! Its really remarkable piece of writing,
I have got much clear idea concerning from this paragraph.
Hello, everything is going perfectly here and ofcourse
every one is sharing information, that’s genuinely good, keep up writing.
Yes! Finally something about winning303.
Way cool! Some extremely valid points! I appreciate
you penning this post and the rest of the site is also really good.
Asking questions are truly nice thing if you are not understanding something entirely, except this piece
of writing gives fastidious understanding even.
Informative article, totally what I was looking for.